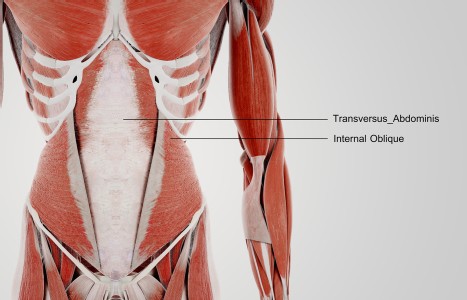
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Herbal Monograph for Xiao Chai Hu Tang
Xiao chai hu tang (Minor Bupleurum Decoction) is one of the most commonly used herbal formulas today. Historically, it was used to treat shaoyang syndrome. Today, it is used to successfully treat many disorders including hepatitis, liver fibrosis, liver cancer, jaundice, cholecystitis, cholelithiasis, pancreatitis, nephritis, acute tonsillitis, parotitis, stomatitis and many more. To achieve optimal therapeutic outcome, it is of critical importance to learn beyond the traditional aspect of this formula. Understanding of topics such as pharmacological effect, clinical studies and research, toxicology and herb-drug interactions will greatly empower the practitioners to properly select the best herbal formula for treatment. Listed below is the herbal monograph on Xiao chai hu tang (Minor Bupleurum Decoction), an excerpt from Chinese Herbal Formulas and Applications by John and Tina Chen, to be published by Art of Medicine Press in fall, 2007.
Xiao Chai Hu Tang (Minor Bupleurum Decoction)
Pinyin Name: Xiao Chai Hu Tang
Literal Name: Minor Bupleurum Decoction
Alternate Names: Hsiao Tsai Hu Tang, Minor Bupleurum Combination
Original Source: Shang Han Lun (Discussion of Cold-Induced Disorders) by Zhang Zhong-Jing in the Eastern Han Dynasty
Composition
| Chai Hu (Radix bupleuri) | 24g [12g] |
| Huang Qin (Radix scutellariae) | 9g [9g] |
| Ban Xia (Rhizoma pinelliae), xi (washed) | 0.5 cup [9g] |
| Sheng Jiang (Rhizoma zingiberis recens), qie (sliced "Slicing") | 9g [9g] |
| Ren Shen (Radix et rhizoma ginseng) | 9g [6g] |
| Zhi Gan Cao (Radix et rhizoma glycyrrhizae praeparata cum melle) | 9g [5g] |
| Da Zao (Fructus jujubae), bo (opened) | 12 pieces [4 pieces] |
Dosage/Preparation/Administration
The source text specifies to cook the ingredients in 12 cups [2400 mL] of water until 6 cups [1200 mL] of the liquid remain. Discard the residue and cook the strained decoction again until it is reduced to 3 cups [600 mL]. Take 1 cup [200 mL] of warm decoction per dose, three times daily. Today, the decoction may be prepared using the dosages suggested in brackets.
Chinese Therapeutic Actions
Harmonizes shaoyang
Clinical Manifestations
- Shaoyang syndrome: alternating spells of fever and chills, chest and hypochondriac fullness and discomfort, irritability, a bitter taste in the mouth, lack of appetite, nausea, vomiting, vertigo, a dry throat, a thin, white tongue coating and a wiry pulse.
- Any of the following disorders with shaoyang characteristics: gynecological disorders with heat in the uterus, liver or chong (thoroughfare) channel; malaria; jaundice; or any internal injury characterized by shaoyang syndrome.
Clinical Applications
Hepatitis, viral hepatitis, chronic hepatitis, hepatic fibrosis and carcinoma, hepatocellular carcinomas, jaundice, cholecystitis, cholelithiasis, pancreatitis, fever, fever in cancer, nephritis, chronic renal insufficiency, acute tonsillitis, infectious parotitis, stomatitis, common cold, influenza, measles, bronchitis, pneumonia, pulmonary tuberculosis, cough, allergic rhinitis, bronchial asthma, reflux esophagitis, antral gastritis, gastritis, gastric pain, gastric prolapse, constipation, Meniere's syndrome, dizziness, seizures, migraine, angina, depression, chronic fatigue syndrome, morning sickness, postpartum infection, postpartum fever, dysmenorrhea, premenstrual syndrome and malaria.
Explanation
Xiao chai hu tang (Minor Bupleurum Decoction) is the main formula for harmonizing shaoyang syndrome, one of the six stages of disease progression described in Shang Han Lun (discussion of cold-induced disorders). The shaoyang is situated between yang and yin, or between the exterior and interior; therefore, alternating spells of fever and chills may occur in shaoyang syndrome if the body is fighting both the pathogens outside and the disharmony inside.
Disorders in the shaoyang might cause qi stagnation and eventual heat formation in the gallbladder channel (a shaoyang channel), giving rise to chest and hypochondriac fullness and discomfort, a bitter taste in the mouth, vertigo, a dry throat and irritability. Lack of appetite, nausea and vomiting are the results of gallbladder heat invading the stomach. The tongue coating is thin and white because the pathogenic factors have not yet transformed into internal heat. The wiry pulse is the result of qi stagnation in the shaoyang channel.
Because the disease resides between the exterior and the interior, it is not suitable to use only exterior-releasing herbs or only purgative herbs. Use of only exterior-releasing herbs will not treat the interior condition, and use of only heat-clearing or downward-draining herbs will bring the pathogens from the exterior into the interior. Therefore, the harmonizing method is the most appropriate treatment approach in this condition.
Chai hu (Radix bupleuri) is the main herb for treating shaoyang disorders. The light quality of chai hu (Radix bupleuri) lifts and disperses stagnation, as well as releases to the exterior. Huang qin (Radix scutellariae), a bitter and cold herb that enters the gallbladder channel, is ideal for clearing shaoyang heat. Together, chai hu (Radix bupleuri) disperses the exterior while huang qin (Radix scutellariae) clears the interior to achieve the harmonizing effect. Ban xia (Rhizoma pinelliae), besides harmonizing the stomach to relieve nausea and vomiting, disperses stagnation in the body. Sheng jiang (Rhizoma zingiberis recens) helps ban xia (Rhizoma pinelliae) harmonize the middle jiao. It also reduces the toxicity of ban xia (Rhizoma pinelliae). Ren shen (Radix et rhizoma ginseng), zhi gan cao (Radix et rhizoma glycyrrhizae praeparata cum melle), and da zao (Fructus jujubae) tonify stomach qi, nourish body fluids and harmonize the ying (nutritive) and wei (defensive) levels. The combination of chai hu (Radix bupleuri) and ren shen (Radix et rhizoma ginseng) also provides a mutual check and balance for each other: chai hu (Radix bupleuri) prevents the tonic effect of ren shen (Radix et rhizoma ginseng) from retaining the pathogens in the body, while ren shen (Radix et rhizoma ginseng) prevents the dispersing effect of chai hu (Radix bupleuri) from damaging qi. Combined, these herbs expel the pathogens and strengthen bodily constitution.
Because the shaoyang stage is unstable and often short and transient, the symptoms listed above may not be clinically present all at the same time. Therefore, as suggested in shang han lun (discussion of cold-induced disorders), this formula can be applied even if there is only one shaoyang symptom clinically present.
| Xiao Chai Hu Tang (Minor Bupleurum Decoction) | |||
| Diagnosis | Signs and Symptoms | Treatment | Herbs |
| Shaoyang syndrome |
| Harmonizes shaoyang |
|
Modifications
General Signs and Symptoms:
- If accompanied by headache, add chuan xiong (Rhizoma chuanxiong).
- If there is thirst, remove ban xia (Rhizoma pinelliae) and add tian hua fen (Radix trichosanthis).
- With thirst and irritability from deficiency in heat, add mai dong (Radix ophiopogonis) and wu wei zi (Fructus schisandrae chinensis).
- If there is no thirst but a slight fever and exterior symptoms are present, remove ren shen (Radix et rhizoma ginseng) and add gui zhi (Ramulus cinnamomi).
- With irritability, add dan zhu ye (Herba lophatheri) and geng mi (Semen oryzae).
- With more irritability but absence of nausea or vomiting, remove ban xia (Rhizoma pinelliae) and ren shen (Radix et rhizoma ginseng) and add gua lou (Fructus trichosanthis).
- With abdominal pain, remove huang qin (Radix cutellariae) and add bai shao (Radix paeoniae alba).
- With more vomiting or nausea, add sheng jiang (Rhizoma zingiberis recens) and chen pi (Pericarpium citri reticulatae).
- When there is indigestion in children, add bai zhu (Rhizoma atractylodis macrocephalae), chen pi (Pericarpium citri reticulatae), fu ling (Poria) and shan zha (Fructus crataegi).
- If there is gum pain caused by yin deficiency, add shi gao (Gypsum fibrosum).
- With palpitations and dysuria, remove huang qin (Radix scutellariae) and add fu ling (Poria).
- With distention and hardness of the hypochondriac area caused by phlegm accumulation, remove da zao (Fructus jujubae) and add mu li (Concha ostreae).
- If the hypochondriac pain is severe, add qing pi (Pericarpium citri reticulatae viride), bai shao (Radix paeoniae alba) and xiang fu (Rhizoma cyperi).
- With a stifling sensation in the chest, add zhi shi (Fructus aurantii immaturus) and qing pi (Pericarpium citri reticulatae viride).
Infectious Disorders:
- For common colds, add jing jie (Herba schizonepetae), fang feng (Radix saposhnikoviae) and ge gen (Radix puerariae lobatae).
- For influenza, add jin yin hua (Flos lonicerae japonicae), lian qiao (Fructus forsythiae) and ban lan gen (Radix isatidis).
- For acute bronchitis, add jie geng (Radix platycodonis), zhi qiao (Fructus aurantii), ku xing ren (Semen armeniacae amarum) and bai bu (Radix stemonae).
- For chronic bronchitis, add fu ling (Poria), chen pi (Pericarpium citri reticulatae), zi wan (Radix et rhizoma asteris) and kuan dong hua (Flos farfarae).
- For acute otitis media, add long dan (Radix et rhizoma gentianae) and zhi zi (Fructus gardeniae).
- For urinary tract infection, add bian xu (Herba polygoni avicularis), che qian cao (Herba plantaginis) and hai jin sha (Spora lygodii).
- For malaria, add chang shan (Radix dichroae), bing lang (Semen arecae) and wu mei (Fructus mume).
Liver and Gallbladder Disorders:
- For icteric jaundice and hepatitis, add zhi shi (Fructus aurantii immaturus), yin chen (Herba artemisiae scopariae), bai shao (Radix paeoniae alba) and jin qian cao (Herba lysimachiae).
- For damp-heat jaundice, add yin chen (Herba artemisiae scopariae), zhi zi (Fructus gardeniae) and ban lan gen (Radix isatidis).
- For jaundice with more heat, add zhi zi (Fructus gardeniae) and huang bo (Cortex phellodendri chinensis).
- For jaundice resulting from hepatitis or cholecystitis, add zhi shi (Fructus aurantii immaturus), yin chen (Herba artemisiae scopariae), bai shao (Radix paeoniae alba) and jin qian cao (Herba lysimachiae).
Gynecological Disorders:
- For postpartum wind invasion with perspiration, remove chai hu (Radix bupleuri).
- For postpartum wind invasion without fever, remove huang qin (Radix scutellariae).
- For postpartum wind invasion with increased vomiting or nausea, increase the dosage of sheng jiang (Rhizoma zingiberis recens).
- For postpartum wind invasion with marked deficiency, increase the dosage of ren shen (Radix et rhizoma ginseng).
- When there is wind invasion during the menstrual period, add niu xi (Radix achyranthis bidentatae), tao ren (Semen persicae) and mu dan pi (Cortex moutan).
Cautions/Contraindications
- Xiao chai hu tang should be used with caution in patients of yin and/or blood deficiencies, in patients of upper excess and lower deficiency, or in patients of liver fire. Inappropriate use of this formula may result in headache, dizziness or bleeding gums.
- In general, there is no sweating associated with relief of symptoms following the administration of Xiao chai hu tang, since it harmonizes, rather than releases the exterior. However, some patients do show sweating prior to recovery. They should be monitored closely to prevent excessive sweating from injuring yin.
- Avoid cold, raw, pungent and spicy foods while taking this formula.1
References
- Zhong Yao Ming Fang Yao Li Yu Ying Yong Pharmacology and Applications of Famous Herbal Formulas, 1989:92-96.
- Yao Xue Za Zhi. Journal of Medicinals, 1984;104(7):798.
- Guo Wai Yi Xue. Foreign Medicine, 1984;(5)279.
- Kusunose M, Qiu B, Cui T, et al. Effect of Sho-saiko-to extract on hepatic inflammation and fibrosis in dimethylnitrosamine induced liver injury rats. Biol Pharm Bull, November 2002;25(11):1417-21.
- Kaneko M, Kawakita T, Tauchi Y, et al. Augmentation of NK activity after oral administration of a traditional Chinese medicine, xiao-chai-hu-tang (shosaiko-to). Immunopharmacol Immunotoxicol, February 1994;16(1):41-53.
- Yamashiki M, Asakawa M, Kayaba Y, et al. Herbal medicine "sho-saiko-to" induces in vitro granulocyte colony-stimulating factor production on peripheral blood mononuclear cells. J Clin Lab Immunol, 1992;37(2):83-90.
- Guo Wai Yi Xue. Foreign Medicine, 1991;13(4):46.
- Guo Wai Yi Xue. Foreign Medicine, 1991;13(4):43.
- Yao Xue Za Zhi. Journal of Medicinals, 1984;104(5):509.
- Zhong Yi Fang Ji Xian Dai Yan Jiu. Modern Study of Medical Formulae in Traditional Chinese Medicine, 1997,(1):184.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1990;11(8):376.
- Gan Su Zhong Yi Xue Yuan Xue Bao. Journal of Gansu University of Chinese Medicine, 1991;8(3):39.
- Zhong Yi Fang Ji Xian Dai Yan Jiu, Modern Study of Medical Formulae in Traditional Chinese Medicine, 1997;(1):186.
- Umeda M, Amagaya S, Ogihara Y. Effect of shosaikoto, daisaikoto and sannoshashinto (traditional Japanese and Chinese medicines) on experimental hyperlipidemia in rats. J Ethnopharmacol, October 1989;26(3):255-69.
- Matsumoto T, Shibata T. The ex vivo effect of the herbal medicine sho-saiko-to on histamine release from rat mast cells. Eur Arch Otorhinolaryngol, 1998;255(7):359-64.
- Matsuta M, Kanita R, Tsutsui F, Yamashita A. Antiulcer properties of shosaiko-to. Nippon Yakurigaku Zasshi, October 1996;108(4):217-25.
- Kase Y, Yuzurihara M, Iizuka S, et al. The effects of hange-shashin-to on gastric function in comparison with sho-saiko-to. Biol Pharm Bull, November 1997;20(11):1155-9.
- Ito H, Shimura K. Studies on the anti-tumor activity of traditional Chinese medicines. (II). The anti-tumor mechanism of traditional Chinese medicines. Gan To Kagaku Ryoho, November 1985;12(11):2149-54.
- Kato M, Liu W, Yi H, et al. The herbal medicine Sho-saiko-to inhibits growth and metastasis of malignant melanoma primarily developed in ret-transgenic mice. J Invest Dermatol, October 1998;111(4):640-4.
- Liu W, Kato M, Akhand AA, et al. The herbal medicine sho-saiko-to inhibits the growth of malignant melanoma cells by upregulating Fas-mediated apoptosis and arresting cell cycle through downregulation of cyclin dependent kinases. Int J Oncol, June 1998;12(6):1321-6.
- Ito H, Shimura K. Effects of a blended Chinese medicine, xiao-chai-hu-tang, on Lewis lung carcinoma growth and inhibition of lung metastasis, with special reference to macrophage activation. Jpn J Pharmacol, July 1986;41(3):307-14.
- Kure F. The radioprotective effects of methylprednisolone and Sho-Saikoto on mouse lung. Nippon Igaku Hoshasen Gakkai Zasshi, Jan. 25 1992;52(1):96-103.
- Nishioka Y, Kyotani S, Miyamura M, Kusunose M. Influence of time of administration of a Shosaiko-to extract granule on blood concentration of its active constituents. Chem Pharm Bull (Tokyo), May 1992;40(5):1335-7.
- Fu Jian Zhong Yi Yao. Fujian Chinese Medicine and Herbology, 1986;17(3):48.
- Shi Yong Zhong Xi Yi Jie He Za Zhi. Practical Journal of Integrated Chinese and Western Medicines, 1993; 4:218.
- Zhong Yi Za Zhi. Journal of Chinese Medicine, 1982;9:40.
- Hirayama C, Okumura M, Tanikawa K, et al. A multicenter randomized controlled clinical trial of Shosaiko-to in chronic active hepatitis. Gastroenterol Jpn, December 1989;24(6):715-9.
- Hu Nan Zhong Yi Za Zhi. Hunan Journal of Chinese Medicine, 1989; 5(3):5.
- Xin Yao Yu Lin Chuang. New Medicine and the Clinical Application, 1982; 4:651.
- Hu Nan Zhong Yi Za Zhi. Hunan Journal of Chinese Medicine, 1987; 3:5.
- Zhe Jiang Zhong Yi Xue Yuan Xue Bao. Journal of Zhejiang University of Chinese Medicine, 1999;3:36.
- Yamashiki M, Nishimura A, Suzuki H, et al. Effects of the Japanese herbal medicine "Sho-saiko-to" (TJ-9) on in vitro interleukin-10 production by peripheral blood mononuclear cells of patients with chronic hepatitis C. Hepatology, June 1997;25(6):1390-7.
- Shimizu I. Sho-saiko-to: Japanese herbal medicine for protection against hepatic fibrosis and carcinoma. Journal of Gastroenterology & Hepatology, March 2000;15 Suppl:D84-90.
- Ono M, Miyamura M, Kyotani S, et al. Effects of Sho-saiko-to extract on liver fibrosis in relation to the changes in hydroxyproline and retinoid levels of the liver in rats. J Pharm Pharmacol, September 1999;51(9):1079-84.
- Oka H, Yamamoto S, Kuroki T, et al. Prospective study of chemoprevention of hepatocellular carcinoma with Sho-saiko-to (TJ-9). Cancer, Sept. 1 1995;76(5):743-9.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1995;2:57.
- Si Chuan Zhong Yi. Sichuan Chinese Medicine, 1986;4(5):36.
- Hu Nan Zhong Yi Za Zhi. Hunan Journal of Chinese Medicine, 1996; 2:32.
- Zhong Yi Fang Ji Xian Dai Yan Jiu. Modern Study of Medical Formulae in Traditional Chinese Medicine, 1997;(1):190.
- Zhong Yi Fang Ji Xian Dai Yan Jiu. Modern Study of Medical Formulae in Traditional Chinese Medicine, 1997;190.
- Shan Dong Zhong Yi Za Zhi. Shandong Journal of Chinese Medicine, 1998;8:359.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1995;6:12.
- Guo Wai Yi Xue Zhong Yi Zhong Yao Fen Ce. Monograph of Chinese Herbology from Foreign Medicine, 1992;4:202.
- Zhong Guo Zhong Xi Yi Jie He Za Zhi. Chinese Journal of Integrative Chinese and Western Medicine, 1992;12(11):686.
- Shi Yong Zhong Xi Yi Jie He Za Zhi. Practical Journal of Integrated Chinese and Western Medicines, 1996;5:312.
- Zhong Yi Za Zhi. Journal of Chinese Medicine, 1983;5:41.
- He Nan Zhong Yi. Henan Chinese Medicine, 1995;4:212.
- Si Chuan Zhong Yi. Sichuan Chinese Medicine, 1995;2:20.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1996;5:33.
- Fu Jian Zhong Yi Yao. Fujian Chinese Medicine and Herbology, 1996;3:36.
- An Hui Zhong Yi Xue Yuan Xue Bao. Journal of Anhui University School of Medicine, 1995;2:35.
- Shan Xi Zhong Yi Xue Yuan Xue Bao. Journal of Shanxi University School of Chinese Medicine, 1999;4:39.
- Shi Yong Zhong Yi Za Zhi. Journal of Practical Chinese Medicine, 1995; 2:27.
- Shi Yong Zhong Xi Yi Jie He Za Zhi. Practical Journal of Integrated Chinese and Western Medicines, 1997;11:1054.
- Shi Yong Zhong Xi Yi Jie He Za Zhi. Practical Journal of Integrated Chinese and Western Medicines, 1996;5:294.
- Guang Xi Zhong Yi Yao. Guangxi Chinese Medicine and Herbology, 1996;3:3.
- He Nan Zhong Yi. Henan Chinese Medicine, 1986;3:18.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1996;2:10.
- He Bei Zhong Yi. Hebei Chinese Medicine, 1998;6:375.
- Shan Xi Zhong Yi. Shanxi Chinese Medicine, 1989;5:203.
- Si Chuan Zhong Yi. Sichuan Chinese Medicine, 1996;10:41.
- Shi Yong Zhong Xi Yi Jie He Za Zhi. Practical Journal of Integrated Chinese and Western Medicines, 1997;19:1927.
- Jiang Xi Zhong Yi Yao. Jiangxi Chinese Medicine and Herbology, 1992;4:39.
- Bei Jing Zhong Yi. Beijing Chinese Medicine, 1987;6:30.
- Nakagawa A, et al. Five patients of drug-induced pneumonitis due to Sho-saiko-to or interferon-alpha or both. Nihon Kyobu Shikkan Gakkai Zasshi, December 1995;33(12):1361-6.
- Murakami K, et al. A possible mechanism of interstitial pneumonia during interferon therapy with sho-saiko-to. Nihon Kyobu Shikkan Gakkai Zasshi, April 1995;33(4):389-94.
- Ishizaki T, Sasaki F, Ameshima S, et al. Pneumonitis during interferon and/or herbal drug therapy in patients with chronic active hepatitis. European Respiratory Journal, December 1996;9(12):2691-6.
- Huang Y, Marumo K, Murai M. Anti-tumor effects and pharmacological interaction of xiao-chai-hu-tang (sho-saiko-to) and interleukin 2 in murine renal cell carcinoma. Keio J Med, Sept. 1997;46(3):132-7.
- Piras G, Makino M, Baba M. Sho-saiko-to, a traditional Kampo medicine, enhances the anti-HIV-1 activity of lamivudine (3TC) in vitro. Microbiology & Immunology, 1997;41(10):835-9.
- Ohta T, Tawara M, Tatsuka M, et al. An approach to prolongation of survival rate in tumor bearing mice using 5-fluorouracil in combination with various kinds of herb medicine. Gan To Kagaku Ryoho, August 1983;10(8):1858-65.
- Mitsukawa H, Ikeda K. Effect of sho-saiko-to (xiao-chai-hu-tang) on hepatic injury induced by halothane in rats. Masui, May 1991;40(5):794-800.
- Yaginuma T, Okamura T, Takeuchi T, et al. Preventive effect of traditional herbal medicine, shosaiko-to, on danazol-induced hepatic damage. Int J Gynaecol Obstet, August 1989;29(4):337-41.
- Ohta Y, Nishida K, Sasaki E, et al. Comparative study of oral and parenteral administration of sho-saiko-to (xiao-chaihu-tang) extract on D-galactosamine-induced liver injury in rats. Am J Chin Med, 1997;25(3-4):333-42.
- Amagaya S, Hayakawa M, Ogihara Y, et al. Treatment of chronic liver injury in mice by oral administration of xiao-chai-hu-tang. J Ethnopharmacol, April 1989;25(2):181-7.
- Saruwatari J, Nakagawa K, Shindo J, et al. The in-vivo effects of sho-saiko-to, a traditional Chinese herbal medicine, on two cytochrome P450 enzymes (1A2 and 3A) and xanthine oxidase in man. Journal of Pharmacy & Pharmacology, November 2003;55(11):1553-9.
- Takahashi K, Uejima E, Morisaki T, et al. In vitro inhibitory effects of Kampo medicines on metabolic reactions catalyzed by human liver microsomes. Journal of Clinical Pharmacy & Therapeutics, August 2003;28(4):319-27.
- Nose M, Tamura M, Ryu N, et al. Sho-saiko-to and Saiko-keisi-to, the traditional Chinese and Japanese herbal medicines, altered hepatic drug-metabolizing enzymes in mice and rats when administered orally for a long time. J Pharm Pharmacol, October 2003;55(10):1419-26.
- Ohnishi N, Okada K, Yoshioka M, et al. Studies on interactions between traditional herbal and western medicines. V. effects of Sho-saiko-to (Xiao-Cai-hu-Tang) on the pharmacokinetics of carbamazepine in rats. Biol Pharm Bull, November 2002;25(11):1461-6.
- American Journal of Chinese Medicine, 1999;27(3-4):355-63.
- Nishimura N, Naora K, Hirano H, Iwamoto K. Effects of sho-saiko-to (xiao chai hu tang), a Chinese traditional medicine, on the gastric function and absorption of tolbutamide in rats. Yakugaku Zasshi, February 2001;121(2):153-9.
- International Journal of Clinical Pharmacology and Therapeutics, February 1994;32(2):57-61.
- Yi Fang Xin Jie. New Explanation for Medical Formulas, 1980;42.
- Liu ZL, Tanaka S, Horigome H, et al. Induction of apoptosis in human lung fibroblasts and peripheral lymphocytes in vitro by Shosaiko-to derived phenolic metabolites. Biological & Pharmaceutical Bulletin, January 2002;25(1):37-41.
- Yamashiki M, Nishimura A, Huang XX. Nobori T. Sakaguchi S. Suzuki H. Effects of the Japanese herbal medicine "Sho-saiko-to" (TJ-9) on interleukin-12 production in patients with HCV-positive liver cirrhosis. Developmental Immunology, 1999;7(1):17-22.
- Wang MZ, et al. Zhong Yi Xue Wen Da Ti Ku. Questions and Answers on Traditional Chinese Medicine: Herbal Formulas.
- Wang MZ, et al. Zhong Yi Xue Wen Da Ti Ku. Questions and Answers on Traditional Chinese Medicine: Herbal Formulas.
- Wang MZ, et al. Zhong Yi Xue Wen Da Ti Ku. Questions and Answers on Traditional Chinese Medicine: Herbal Formulas.
Editor's Note: Part 2 of this article will appear in the August 2007 issue of Acupuncture Today.