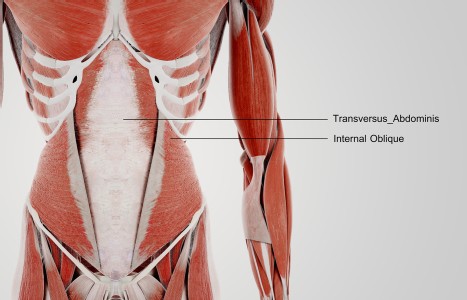
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Compassionate ABT for Palliative Care
Working with a client through pregnancy labor, delivery, and any postpartum challenges, offers an incredible learning experience no textbook or workshop could possibly match. Similarly, if you have a chance to work with a client, friend or family member during a very different sort of transition at the end of life, the experience is profound. It takes time and the subtle art of "tuning in." No two births are alike. Similarly, no two deaths are alike.
I am currently pioneering CEU workshops in ABT for Palliative Care in Europe and the U.S. It's illumining to see how participants react. Some fearful, some tearful. So we start on a practical note. I break them into smaller groups to discuss the most helpful and least helpful experiences they have encountered when navigating the death of a loved one. This prompts everyone to hunker down and discuss many of the reasons why they were in my workshop.
One participant was still trying to process her young brother's suicide and the guilt trips her parents placed on her. Another was dealing with the slow decline of her mother. One praised Hospice care and support. Others spoke about the comfort of appropriate rituals in processing death, regardless of the religious belief system. Some resented friends who tried to impose rigid belief systems or chant inappropriate mantras around a deathbed. Others resented family members who did nothing to help. Others emphasized the vital role children and pets play as a balancing factor during a time of loss. Several described the comfort found in art, music, and some sense of continuity or connectedness with a loved one through meditation or ritual. Awareness of all of the above is essential for a therapist.
Be Prepared for Everything
We discuss Shiatsu's multi-layered role and the minimalist art of tuning into clients' specific physical and emotional needs and mood swings through transitions. We discuss family dynamics surrounding a dying client, or a grieving client. "Don't be thrown if you witness a family argument around a deathbed," I tell them. "Stay in your Qi. Try to move the noise outside to the waiting area." Families should never assume that someone in a coma can't hear what's going on.
In short, I tell them, prep yourselves for everything. Don't approach bedsides with a long face or show any uncertainty or fear, because that will only unsettle – or annoy - your client. Sometimes dying clients can express a lot of frustration and rage, often reflecting their subconscious way of separating themselves to make the eventual departure less painful. Feel free to leave the room when necessary for fresh air and tea. Don't lose your Qi space. And never forget your sense of humor. I learned a lot from Sister Loretta, a Cabrini Hospice nun in New York. Knowing that many terminally ill patients suffer from insomnia, she wisecracked her way around the Hospice beds at night dressed as a clown to interact with anyone who wanted to talk, be they Catholic, Muslim, Jewish, Buddhist or Atheist.
If you know your client well, minimize fussy diagnostic techniques. In a hospital setting, be as subtle and non-invasive as possible and provide simple explanations to any attending MD or RN when necessary. Teach your client's family members easy techniques or basic footwork, for something helpful to do at a loved one's bedside for hours or days.
Focus On A Few Key Points
Concentrate on the most accessible points to ease pain, namely, LI 4, St 36, LIV 2&3, BL 10, GB 20, GB 21. To ease anxiety and fear, let your fingers descend as gracefully as a butterfly onto your client's HC 6 and HC 8. Resting your fingertips gently on GV (Du) 20 is equally calming.
To ease stiffness and prevent bedsores, thumbing down the entire Bladder meridian in the side position works wonders. To ease constipation, LI 4 and St 36 are helpful, along with a rolling technique around the Hara - if that is possible – and also, thumb the sacrum. If you can transfer a client to a chair or wheelchair, ten or fifteen minutes of neck, head and shoulder work helps relieve upper body tension and pain.
Beyond these basic tips, be open. Prepare yourself for the unexpected, especially if you are there during the actual passing, which could be quiet and peaceful, or disturbingly graphic. Be very conscious of body temperature and an increasing coldness or heaviness as Qi starts to transform. Be reassuring in tone and touch. Trust your intuition.
Case Studies
Martha W. of New York was a feisty journalist I treated through months of terminal breast cancer, until I spent one entire Christmas Day at her Hospice bedside in New York City, as she drifted in and out of a coma. I placed a red rose in her line of vision so she could see it each time she opened her eyes. As she was on oxygen and various drips and a catheter, I had to navigate a careful route around her bed.
My aim was just to give comfort, mainly holding points on her hands and feet, and talking to her even when she wasn't communicating verbally. The sense of hearing is always the last to go. She died two days later. My time with her was a gift for us both. Yes, we had discussed death some weeks beforehand, when she toyed with the idea of hiking off into a remote New England forest to die in the fall foliage. "Oh, very romantic," I said, "but, practical? Comfortable? I don't think so," and we laughed. She didn't have a cozy relationship with family members, but I was the outsider, so she found it easy to talk to me. Raised Jewish, Martha was immersed in a sense of the "here and now" but also, as an independent liberal thinker, she felt there was something more. She grappled intellectually with what lay ahead. "Come on Martha, you're a gifted journalist," I reminded her. "Don't you think they're lining up assignments for you on the other side?" She loved the idea and it helped ease those final weeks.
Billy D. died young of AIDS in Dallas. He was a trainer at a neighborhood gym I attended. Through Billy, I worked with a group of bodybuilders who were all HIV+, all determined to maximize diet and exercise regimens to maintain a quality of life. It wasn't easy to watch Billy decline over a matter of months. In his final weeks, even when he couldn't recognize any of us, he always responded to the touch of Shiatsu, turning on his side and smiling when I approached so I could work on his back to ease stiffness and constipation.
Georgette R. died in London, England, of lung cancer. I sat by her bedside for days. When she started to cough and choke I would point my index fingers and Qi directly at her Lung 1 points. Her spasms would ease within seconds. As she found even the lightest touch around her torso and back uncomfortable, I concentrated on her feet and hands as she drifted in and out of hallucinatory imagery. Many palliative care physicians in Britain learn a very simple form of acupuncture to help relieve pain and discomfort. When I had to return to the U.S., Georgette's physician was very open to my suggestions to needle LI 4 and ST 36 to ease morphine-induced constipation. On my last morning, Georgette turned, gazed out of the window and said, "oh, look at those lovely frisky horses!" There were no horses outside, but the image had a beautifully calming effect. I let my imagination fly along with her.
Pam welcomes your comments. Email her at Pamelacudot@gmail.com