The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
Common Disorders of the Temporomandibular Joint
The evaluation and management of craniofacial pain is a complex endeavor, which often encompasses the presence of temporomandibular joint disorders. There has been much confusion in regard to the differential diagnosis of a TMJ Disorder; however, this confusion can be easily clarified. The need for clarity is necessary for any practitioner who attempts to treat these disorders either individually or as part of a team in a multidisciplinary approach.
Temporomandibular Joint Disorders (TMJD) has been included in the more encompassing term of Temporomandibular Disorders (TMD). There are four common occurrences that manifest in the temporomandibular joint and surrounding anatomical areas. The first of those clinical phenomena are inflammatory disorders, specifically synovitis, capsulitis and retrodiscitis.
The second clinical occurrence concerns the presence of internal structural changes, which may be present within the joint itself; these are referred to as an internal derangements. The third clinical situation includes the musculature of the masticatory system, particularly the muscles which are responsible for elevating or closing the mandible. These are considered extracapsular in nature. The fourth common clinical occurrence is considered a hypermobility of jaw movement and is termed a dislocation. The fifth possible clinical scenario entails the presence of degenerative changes. These various disorders rarely manifest as singular entities, and in many cases can occur together.
Capsulits And Synovitis
Capsulitis and synovitis are hard to differentiate clinically and are usually concomitant occurrences. A capsulitis is technically an inflammation of the outer fibrous layer of the joint capsule and a synovitis is an inflammation of the inner synovial lining. Trauma is the usual cause of capsulitis/synovitis, which can occur from hard chewing, grinding of the teeth (bruxism), clenching or from external trauma.
The main finding is that there is pain at rest, which is exacerbated with movement such as chewing or talking. There may be limitation of mandibular movement or increased pain as the normal range of motion is achieved. Clinically, there is pain in response to palpation in front of the ear, the area at the outside or lateral aspect of the temporomandibular joint.
Retrodiscitis
A retrodiscitis occurs when there is an inflammatory response in the posterior part of the joint in the area where there is an abundant blood and nerve supply located posterior to the articular disc. An acute traumatic episode is usually the cause of the retrodiscitis. A dental malocclusion when there is an inadequate molar support can also predispose an individual to this kind of clinical situation.
When a retrodiscitis occurs clinically, the following is usually observed. If there is a one-sided occurrence, there will be pain with closure on the affected side and the mandible will usually move or shift to the contralateral side. There will be premature contact of teeth on the opposite side and there may be little or no contact on the side of the inflammation where a retrodiscitis is present.
If there is a bilateral retrodiscitis, the entire mandible will move forward and there will be contact solely on the anterior teeth. There should be no attempt to try to force the mandible back when this is present. Conservative measures to decrease the inflammatory process are the initial steps necessary in all cases when a retrodiscitis is present.
Internal Derangements (Intracapsular Structural Changes)
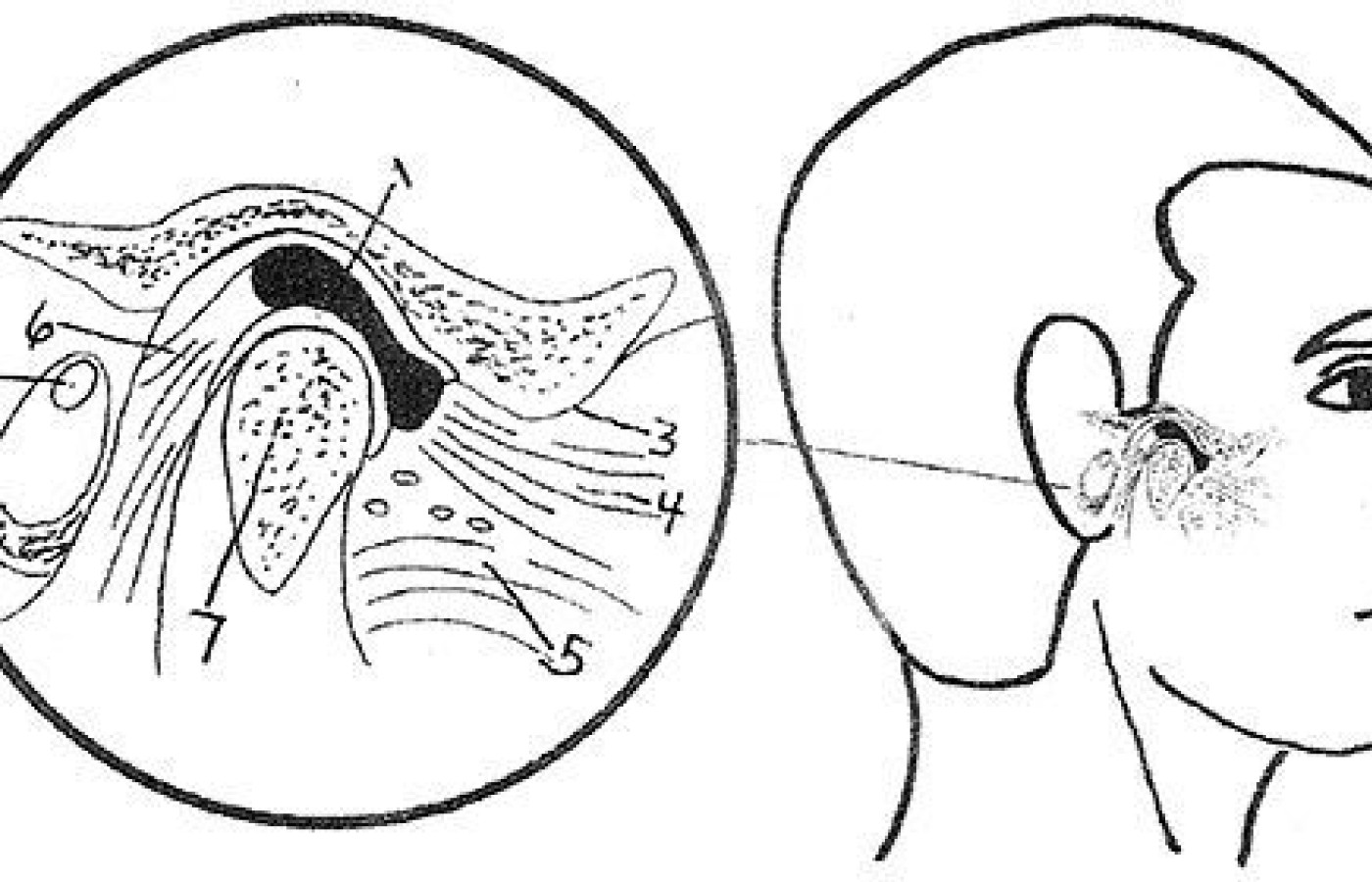
There are structural changes that can occur within the temporomandibular joint. There can be a displacement of the disc, which is composed of fibro-cartilage. This displacement is termed an internal displacement. The disc can become displaced in an anterior, medial, lateral or posterior direction. The most common internal derangement is an anteriorly displaced disc. This will manifest clinically with clicking with opening and the mandible may move to the affected side with opening movement. This movement is termed a deviation. The earlier a click occurs when opening the less the disc has moved out of position.
Conversely, the later a click occurs with opening, the greater the displacement and the more severe the case. An internal derangement can be present on one or both sides. The technical term for this kind of internal derangement is an anterior disc displacement with reduction. The term reduction refers to the repositioning of the disc back on top of the condyle with opening when this occurs, a click can be observe audibly or by palpation in front of the ear. A stethoscope can be utilized for this purpose as well.
Another internal derangement, which is more severe than the clinical situation previously mentioned if referred to as a closed lock or anterior medial disc displacement without reduction. In this case, the articular disc is more severely displaced in the closed position that does not reduce or reposition itself upon opening. There is limitation of opening and the mandible usually moves to the side of the displacement. This movement to the affected side is call a deflection. A closed lock can occur in both temporomandibular joints simultaneously or it can occur unilaterally.
Clicking will not occur with a closed lock. In obtaining a history, clicking proceeds the occurrence of the closed lock and the patient is usually able to pinpoint the exact time it occurred. A closed lock can be experienced with or without pain.
Myofascial Trigger Points
Myofascial trigger points are localized areas of hypersensitivity that are found in muscle tissue, tendons, ligaments and periosteum. These areas are found to be tender when palpated and they can also refer pain to other areas, which are usually along acupuncture pathways. In Traditional Chinese Medicine, trigger points (considered areas of blood stasis and constrained qi) are called ashi points. The normal functions of many of the systems of the body, particularly the muscular, nervous, lymphatic and circulatory systems are particularly affected by the presence of these localized areas of hypersensitivity.
Some of the common areas where trigger points occur are in the face, head and cervical area; and posterior cervical muscles. The masseter muscle is one of four elevator or closing muscles of the mandible. This is the area where the stomach meridian transverses and is also a viscero-somatic correspondence point, which can be an indication of protein deficiency.
Muscle Spasm
Muscle spasm is an acute occurrence where a muscle or a number of muscles contract, causing limitation of motion and discomfort. From a dental perspective, this can occur from a prolonged dental appointment where the mouth was opened for an extensive period of time or from a mandibular block injection. This is referred to as trismus. It is mandatory to employ stretching exercises or utilization of a mechanical self-help device to establish normal muscle function after an episode of this nature.
Excessive Anterior Movement of the Disc and Condyle Hypermobility
There can be excessive movement of the disc and condyle beyond normal limits. When the disc and condyle move behind the articular eminence, a condition known as a hypermobility exists. While this is not considered an internal derangement, this is a district clinical entity where there is a dysfunction within the temporomandibular joint. This has also been referred to as a partial dislocation. When a hypermobility occurs, a discernible noise or "pop occurs and the mandible moves to the unaffected side with opening. A hypermobility can be present bilaterally as well.
Dislocation
A dislocation can occur when a hypermobility has been present for along time. This can also occur after extreme mouth opening or yawning. A dislocation is referred to as an "open lock." There is an inability to close; the mouth is stuck in a position where there is an inability to achieve full closure. Manipulation techniques can be attempted to address a dislocation. However, in many cases, intravenous sedation is required before a successful attempt to reduce the dislocation is pursued.
Degenerative Changes
There are a number of degenerative diseases that can occur in the temporomandibular joint. These degenerative changes primarily affect the articular (bony) surfaces of the internal structures of the temporomandibular joint. There are systemic and localized disorders that can affect the articular surfaces.
There are two localized conditions that are commonly found; osteoarthritis and osteoarthrosis. When osteoarthritis is present, there is an inflammation of the synovial lining of the temporomandibular joint which elicits pain. Pain is usually constant and increases with function. In many cases, there are structural osseous charges, particularly in the condyle or fossa. In many instances, pain is self-limiting and the status of a joint is considered an osteoartrosis, which is a manifestation of degenerative joint disease without the presence of inflammation. There may be limitation of mandibular motion and a grating, cracking sound may originate in the joint with movement which is known as crepitus.
The preceding is an overview of common TMJ disorders that are present in patients in all health care practices throughout the world. Acupuncture and Oriental Medicine protocols have proven invaluable in managing many of these cases. It is, however, mandatory to know what kind of disorders that present clinically. For example, acupuncture is not effective in resolving a closed lock (anterior medial disc displacement without reduction). It is very important to know what disciplines will be effective in providing appropriate treatment. In the realm of TMJ disorders, it is extremely important to be able to make the differential diagnosis that has been previously outlined in this article.
Resources:
- Pertes, Richard, DDS, and Gross, Sheldon G, DDS, Clinical Management of Temporomandibular Disorders and Orofacial Pain, 1995, Hanover Park, Il: Quintessence Publishing
- Bell, Welden E, Orofacial Pains- Classification- Diagnosis Management, 4th Edition 1989
- Kaptchuck, Ted J., OMD, The Web That Has No Weaver, Understanding Chinese Medicine, 2000, New York, NY; McCraw-Hill
- Kessler, Carol S., PhD, LAc, MS, LMT, and Mark, Barry M., DDS, LAc, CAc, Hom, All Pain Is Not The Same- A Unique Perspective on Headaches, TMJ Disorders, and Facial Pain, 2010, Lobelville, TN, JimSam, Publishing, Inc.