The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
The Interstitium and the Eight Extraordinary Vessels, as Taught by Wang Ju-Yi
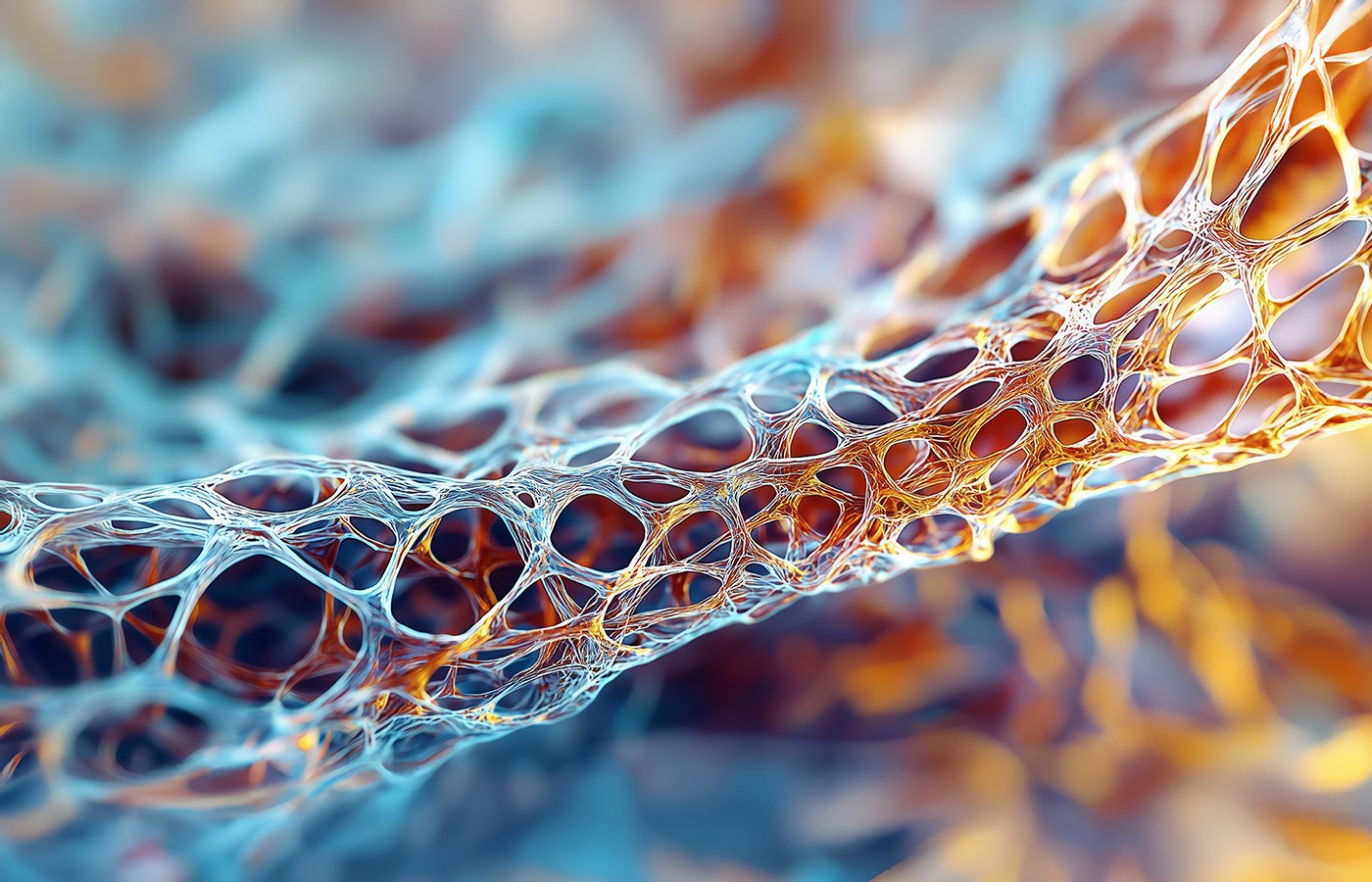
To paraphrase the Tao de Jing; a bowl is useful because of the empty space. Recent anatomical research uncovered evidence for previously undescribed large-scale pathways that span organs, blood vessels and other connective tissue. These pathways are defined by what is known as the interstitial space between cells. This space, which has been long known and utilized therapeutically, refers to the space between cells. The newer research provides evidence that these interstitial spaces actually make very large-scale networks between different types of tissue.
Despite cultural, intellectual and theoretical differences, healing traditions all work with the human body. The book Applied Channel Theory in Chinese Medicine1 presents clear and detailed information from Dr. Wang Ju-Yi's long and distinguished career as an acupuncturist in Beijing. He emphasizes channel palpation and classical channel theory, working to reinvigorate modern clinical practice. The sections covering the Extraordinary Vessels offer a fascinating interpretation of this intriguing yet mysterious aspect of Chinese medicine. Ju-Yi goes as far as defining the extraordinary vessels in terms of interstitium:
By narrowing the definition of the extraordinary vessels to the concept of interstitial fluid movement, one can see how they are both different from the twelve regular channels and how they act as reservoirs without definable pathways. … It is these fluids which co mingle with the blood through vessel walls and act as reservoirs of qi constantly interacting with the twelve regular channels.
The eight Extraordinary Vessels represent an aspect of Chinese medicine that has not fit neatly into modern standardization. Nevertheless, they represent a fundamental aspect of the Eastern understanding of the body. The recent anatomical discoveries of large-scale interstitial networks support Ju-Yi’s supposition that the interstitial spaces play a deep regulating role in our bodies. He offers a metaphor to further clarify:
[Once] again a metaphor may be helpful. While the twelve regular channels may be thought of as streams passing between mountain ranges, extraordinary vessels may be likened to a wetland reservoir lying in the lowlands. In the spring when the streams are full, the wetlands absorb the overflow of water. In times of drought, on the other hand, the wetlands act as a source for filling the streambeds with needed water. Throughout the year the water in the streams and all of its living organisms constantly interact with the wetland.
He goes on to specifically cite the role of the Extraordinary Vessels in chronic conditions.
Over time the blockage of qi flow along a regular channel may lead to physiological ‘ruts’ outside the normal channel physiology. That is to say, if a person has a chronic issue that has led to consistently abnormal flow of qi and blood such that it now affects the extraordinary vessels, then it may be difficult to re-establish normal channel circulation. Simply removing the blockage of qi and/or blood from the regular channel is sometimes not enough.
Ju-Yi then offers clinical examples of these types of chronic conditions that called for a diagnosis based on the extraordinary channels. With these excerpts in mind from Wang Yuji, let's consider a more biomedical perspective from Tuckey, the teacher of a style of osteopathic bodywork called counterstrain. While the intellectual frameworks and cultural histories differ quite significantly, both of their clinical approaches emphasize palpation for their assessments, so in a sense they actually have similar perspectives.
Tuckey’s 2021 publication, titled: Impaired Lymphatic Drainage and Interstitial Inflammatory Stasis in Chronic Musculoskeletal and Idiopathic Pain Syndromes: Exploring a Novel Mechanism, leads with the following abstract:2
A normal functioning lymphatic pump mechanism and unimpaired venous drainage are required for the body to remove inflammatory mediators from the extracellular compartment. Impaired vascular perfusion and/or lymphatic drainage may result in the accumulation of inflammatory substances in the interstitium, creating continuous nociceptor activation and related pathophysiological states including central sensitization and neuroinflammation. (Emphasis added)
Here with significant crossover, both clinicians consider the dynamics of the interstitial space in relation to blood fluid flow. To use Ju-Yi’s metaphor, impaired vascular perfusion and/or lymphatic drainage leads to blockages dysregulating the relationship between the wetlands and stream, resulting in perhaps unhealthy stagnation or lack of general flow.
Tuckey argues that this lack of exchange keeps inflammatory molecules in the interstitium, which excessively stimulates the immune and nervous system, leading to a positive feedback loop and chronic disease. He goes on to highlight the specific cytokines and other inflammatory molecules involved.
Cytokines such as TCF-B1 stimulate fibroblasts, the primary builders of fascial connective tissue, to convert into myofibroblasts and increase production of the extracellular matrix, leading to fibrosis.3 This fibrosis and extra contractility from the myofibroblasts are hypothesized by Tuckey, et al., to disrupt pre-lymphatic/interstitial flow through partial or total occlusion.
These shared ideas about regulating the flow and state of interstitial fluids in chronic conditions offer clinical inspiration. Renewed focus and creativity regarding the extraordinary vessels may be warranted in chronic inflammatory conditions. Contemporary biomedical research on the interstitium serves as an example on how research can lead us closer to older understandings about essential aspects of human physiology.
References
- Wang J, Robertson JD. Applied channel theory in Chinese medicine: Wang Ju-Yi’s Lectures on Channel Therapeutics. Eastland Press, 2008.
- Tuckey B, Srbely J, Rigney G, et al. Impaired lymphatic drainage and interstitial inflammatory stasis in chronic musculoskeletal and idiopathic pain syndromes: exploring a novel mechanism. Front Pain Res, 2021;2:691740.
- Kendall RT, Feghali-Bostwick CA. Fibroblasts in fibrosis: novel roles and mediators. Front Pharmacol, 2014 May 27;5:123.