One of the longest nerves in the body is known as the vagus nerve (VN). The VN is the 10th pair of cranial nerves that originates at the brain stem in the medulla oblongata. This nerve is part of the parasympathetic nervous system, which is a part of the ANS. Research suggests ear acupuncture can activate the VN.
The Emerging Role of Nicotine in the Integrative Treatment of Long COVID
- Among the more unconventional options for treating long COVID, nicotine – delivered via low-dose transdermal patches – has surfaced as a potential integrative tool.
- It appears that nicotine competes with spike proteins at the receptor sites, “crowding out” the spike proteins and returning homeostasis (with a minor buzz).
- The absence of randomized, controlled trials (as of February 2025) leaves us reliant on case reports and patient narratives – valuable, but not definitive.
Long COVID, a perplexing constellation of symptoms persisting weeks to months after acute SARS-CoV-2 infection, has challenged conventional medical paradigms. Affecting an estimated 10-30% of those infected with COVID-19,1 it manifests as fatigue, cognitive impairment (“brain fog”), dyspnea, and autonomic dysfunction, including postural orthostatic tachycardia syndrome (POTS).2
There is a growing need for therapies that bridge standard pharmacology with integrative strategies. Among the more unconventional options, nicotine – delivered via low-dose transdermal patches – has surfaced as a potential tool. While the idea may sound wacky, emerging evidence and clinical anecdotes suggest that nicotine warrants further exploration, provided it falls within our professional scope of practice. (Over-the-counter nicotine gum is also an option; however, it doesn’t provide the slow, steady release of nicotine that patches offer. Additionally, there are currently are no studies evaluating nicotine gum as a delivery method for long COVID.)
It is important to recognize the potential risks. Even at low doses, nicotine carries a risk of addiction. As a stimulant and vasoconstrictor, nicotine may worsen certain conditions. Exercise particular caution when considering nicotine therapy for patients who are former smokers.
Understanding Long COVID and the Autonomic Link
The pathophysiology of long COVID remains multifactorial and complex, involving persistent immune activation, neuroinflammation, mitochondrial dysfunction, and autonomic nervous system (ANS) dysregulation.3-4 Several studies have demonstrated the presence of functional autoantibodies targeting G-protein-coupled receptors (GPCRs), contributing to the autonomic instability often seen in POTS and other dysautonomias.5
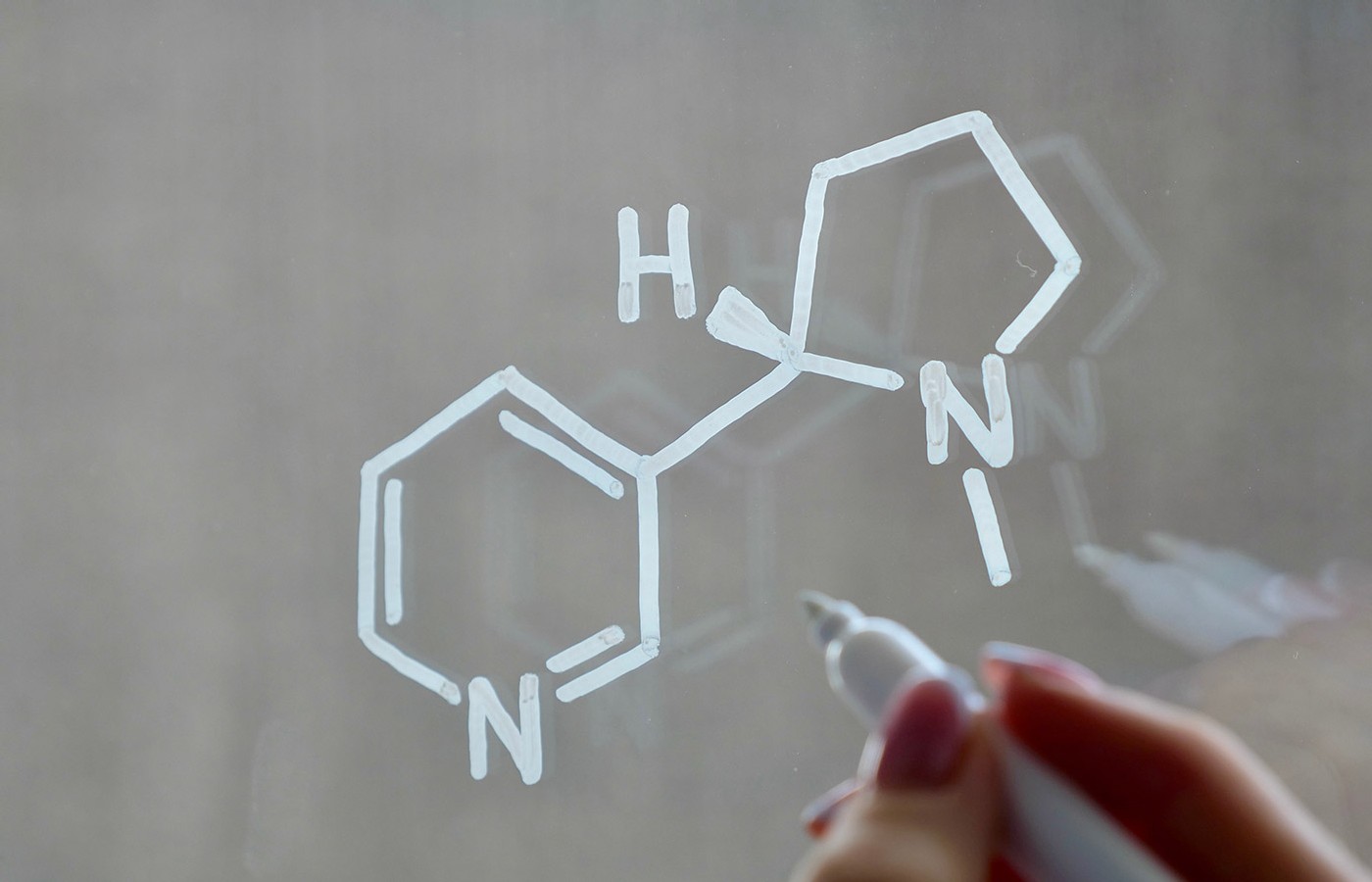
A growing body of research also suggests that SARS-CoV-2 may directly interfere with nicotinic acetylcholine receptors (nAChRs) – key regulators of inflammation, neural signaling and autonomic tone.6 These findings have led to renewed interest in nicotine’s therapeutic potential, particularly via transdermal delivery.
Nicotine’s Mechanistic Rationale
Though historically maligned due to its association with smoking, nicotine in isolation is a pharmacologically active compound that modulates the cholinergic anti-inflammatory pathway, involved with SARS-CoV2 entry and/or replication.7 Specifically, it acts as an agonist at the α7 subtype of nAChRs found on immune and neural cells, inhibiting the release of pro-inflammatory cytokines such as TNF-α and IL-6.8-9 This effect, originally characterized in sepsis and inflammatory disease models, may have relevance in the chronic inflammatory environment of long COVID.
Researchers believe nicotine is involved with inhibiting SARS cov2 cellular entry and/or replication. Since nicotine has a 30 times greater “affinity” than acetylcholine to ACE2 receptors, they “kick off” the spike proteins from the cells, which may lead to short term symptom intensification, but can downregulate sympathetic nervous system activity in the process.
A 2023 case series published in Bioelectronic Medicine described four patients with persistent post-COVID symptoms who were treated with low-dose transdermal nicotine (7.5 mg/24 hr).10 Patients reported improvements in fatigue, cognitive clarity and shortness of breath – often within 48–72 hours of initiating therapy. Although preliminary and uncontrolled, these findings are consistent with anecdotal reports from patient forums and health care professionals.
Clinical Observations
In my own clinical experience, nicotine’s mechanism of action complements acupuncture’s ability to modulate autonomic balance through the vagus nerve. Acupoints such as PC 6 (Neiguan), ST 36 (Zusanli) and auricular Shenmen have been shown to activate brain regions associated with parasympathetic function and stress modulation.11 When layered with transdermal nicotine – particularly in patients with refractory fatigue and dysautonomia – the therapeutic effect may be enhanced.
This synergistic model is not unlike our broader integrative strategies: combining dietary, herbal/vitamin and mineral supplementation, and manual approaches to restore homeostasis. A low-dose nicotine protocol (3.5–7 mg/day) could be paired with:
- Acupuncture: weekly sessions targeting vagal and autonomic acupoints (PC 6, CV 17, auricular Shenmen)
- Magnesium repletion: 200–400 mg/day orally or via transdermal application to support neuromuscular regulation, nerve transmission and vasomotor tone.12-13
- Nutritional support: omega-3 fatty acids, turmeric and a low-histamine diet to further reduce neuroinflammation
Evidence and Limitations
Critics rightly point to the potential for nicotine to exacerbate tachycardia – a core issue in POTS, as well as its addictive potential.14 However, when administered judiciously and at low doses in non-smokers, the risk of dependence is low, particularly with short-term use under clinical supervision.15 The side effects – typically nausea, skin irritation or insomnia – are manageable and reversible upon discontinuation.
Interestingly, early in the pandemic, researchers noted a paradoxical underrepresentation of smokers among hospitalized COVID-19 patients. A systematic review in Nicotine & Tobacco Research highlighted this phenomenon, suggesting potential protective effects of nicotine against SARS-CoV-2 entry or replication.16 While smoking is certainly not advised, it raises important questions about nicotine’s immunomodulatory properties.
Unfortunately, we lack robust randomized, controlled trials evaluating nicotine in long COVID, leaving clinicians to rely on preclinical models, case report, and informed experimentation. Still, this is not without precedent. Nicotine has been studied in other autoimmune and inflammatory contexts – such as ulcerative colitis – with beneficial outcomes.17
The Road Ahead
The value of transdermal nicotine or nicotine gum in long COVID treatment is an exciting proposition ... promising, yet unproven. Its integrative appeal lies in addressing inflammation and autonomic dysfunction, areas in which conventional options often lag. However, without RCTs, it remains experimental; best reserved for cases unresponsive to standard care. As practitioners, we must balance innovation with caution, grounding novel therapies in patient safety and basic principles. Lingering questions include:
- How long should we recommend nicotine administration?
- What’s the “sweet spot” for dosing in milligrams per kilogram of body weight?
- What blood work, lab tests or other measures can be used beyond subjective feedback from our patients to measure their recovery?
For now, nicotine patches offer a curious footnote in the long COVID story – one that challenges us to rethink old tools for new problems. As research evolves, so too will our understanding of where it fits in our clinical arsenal.
References
- Mandel H, Yoo Y, Allen A, et al., Long COVID incidence in adults and children between 2020 and 2023: a real-world data study from the RECOVER Initiative. Research Square [Preprint], 2024 Apr 26:rs.3.rs-4124710.
- Mallick D, Goyal L, Chourasia P, et al. COVID-19 induced postural orthostatic tachycardia syndrome (POTS): a review. Cureus, 2023 Mar 31;15(3):e36955.
- Komaroff AL, Bateman L. Will COVID-19 lead to myalgic encephalomyelitis/chronic fatigue syndrome? Front Med, 2021;7:606824.
- Fernández-Castañeda A, Lu P, Geraghty AC, et al. Mild respiratory SARS-CoV-2 infection can cause multi-lineage cellular dysregulation and myelin loss in the brain. Cell, 2022;185(14):2452-2468.e16.
- Wallukat G, Hohberger B, Wenzel K, et al. Functional autoantibodies against GPCRs in patients with persistent post-COVID-19 symptoms. Front Neurol, 2022;13:840198.
- Tizabi Y, Getachew B, Copeland RL, Aschner M. Nicotine and the nicotinic cholinergic system in COVID-19. FEBS J, 2020 Sep;287(17):3656-3663.
- Wang H, Yu M, Ochani M, et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature, 2003;421(6921):384-388.
- Pavlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Rev Endocrinol, 2012;8(12):743-754.
- Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol, 2010;50:57-81.
- Leitzke M. Is the post-COVID-19 syndrome a severe impairment of acetylcholine-orchestrated neuromodulation that responds to nicotine administration? Bioelectron Med, 2023;9(1):3.
- Zhang Q, Gong J, Dong H, et al. Acupuncture for chronic fatigue syndrome: a systematic review and meta-analysis. Acupunct Med, 2019 Aug;37(4):211-222.
- Gröber U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients, 2015;7(9):8199-8226.
- Reddy B. “Achieving Optimal Health Through Transdermal Magnesium Therapy.” Acupuncture Today, July 2012.
- Benowitz NL, Burbank AD. Cardiovascular toxicity of nicotine: Implications for electronic cigarette use. Trends Cardiovasc Med, 2016 Aug;26(6):515-23.
- De Biasi M, Dani JA. Reward, addiction, withdrawal to nicotine. Annu Rev Neurosci, 2011;34:105-130.
- Usman MS, Siddiqi TJ, Khan MS, et al. Is there a smoker’s paradox in COVID-19?BMJ Evid-Based Med, 2021;26:279-284.
- Kannichamy V, Antony I, Mishra V, et al. Transdermal nicotine as a treatment option for ulcerative colitis: a review. Cureus, 2020 Oct 22;12(10):e11096.