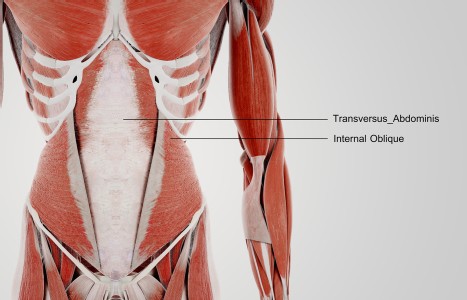
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Official COVID-19 Clinical Guidelines From the Association of Korean Medicine (Pt. 1)
We are facing our biggest challenge of the century with the current COVID-19 pandemic. As we in the U.S. have been struggling with changes and challenges that have impacted every aspect of life, national health organizations in both China and South Korea have been actively engaged in saving the lives and the health of their own citizens – not only with Western medicine, but also with aggressive and active use of TCM modalities, including formulas and acupuncture.
Currently, while official guidelines based on clinical trials are not yet available from any countries, official guidelines from expert consensus are available from China and South Korea. This article fills an important gap by introducing South Korea's national, official clinical strategies for using traditional Asian medicine for COVID-19.1 We hope this information is important and useful, as we are all aware that South Korea is one of the few countries that have been largely successful in containing the spread of COVID-19, and has also been open and honest about the information it provides to its citizens and to the world.

We feel, therefore, that it is extremely meaningful and timely to introduce South Korea's official clinical guideline for COVID-19 from its national organ, the Association of Korean Medicine.2 One of the most important aspects of this guideline is that it is published in an official document by and for professional traditional Asian medicine practitioners (KMDs) in South Korea.
We should also note that the most commonly used Chinese herbal prescription for confirmed cases in China and Korea is Qing Fei Pai Du Tang (Clear the Lungs and Detox Decoction). In addition, South Korea's clinical guideline offers viable herbal formulary options based on differential diagnosis and symptoms of individual patients.
It is important for us to take careful note of what herbal remedies are recommended for preventive measures during the pre-diagnosis stage, the early developmental stage, as well as in recommendations for recovery. For these stages, application of Qing Fei Pai Du Tang is generally not suitable. South Korea's guideline recommends various herbal prescriptions based on differential diagnosis. Huo Xiang Zheng Qi San (Agastache Powder to Rectify Qi) is noteworthy in its use for specific symptoms related to digestive issues.
The clinical guidelines from South Korea were created for Korean medicine doctors who are implementing medical care in national health centers, Korean medicine clinics, traditional Korean medicine hospitals and general hospitals, and specialized general hospitals in charge of primary patient care. The herbal formulas used in the guidelines are those within South Korea's health insurance system. The first edition appeared on March 4, 2020; the second edition was published on March 14, 2020.
The following is a translation of Chart 3 on pp. 23-24, highlights of South Korea's Clinical Guidelines.3 When appropriate, we have added brief comments for either unusual or less-well-known herbal formulas, or formulas that are specifically from traditional Korean medicine herbal classics. [Comments are indicated by a different text appearance and/or set off as Authors' Commentaries.] We have also added organizational structure to the guideline for the purpose of clarification.
1. Prevention With Herbal Medicine (Adults)
During the COVID-19 pandemic, for the maintenance of respiratory health, consider Lian Qiao Bai Du San (Forsythia Power to Overcome Pathogenic Influences) plus Bu Zhong Yi Qi Tang (Tonify the Middle and Augment the Qi Decoction) or Lian Qiao Bai Du San plus Sheng Mai San (Generate the Pulse Powder).
Clinical considerations: High-risk groups, and also for the maintenance of respiratory system health for those that may come in contact with patients with confirmed COVID-19:
- Qi Deficiency: Lian Qiao Bai Du San (Forsythia Power to Overcome Pathogenic Influences) plus Bu Zhong Yi Qi Tang (Tonify the Middle and Augment the Qi Decoction)
- Body Fluid (jin ye) Deficiency: Lian Qiao Bai Du San plus Sheng Mai San (Generate the Pulse Powder)
2. Observational Phase for Patients with Possible Infection (Adults)
For adult patients who have come in contact with COVID-19-confirmed patients, but are asymptomatic, consider Lian Qiao Bai Du San plus Bu Huan Jin Zheng Qi San (Rectify the Qi Powder Worth More Than Gold) or Lian Qiao Bai Du San plus Bu Zhong Yi Qi Tang (Tonify the Middle and Augment the Qi Decoction)
Clinical considerations: For those who have come in close contact with those who are in self-quarantine or with those who have been confirmed:
- Asymptomatic: Use Lian Qiao Bai Du San plus Bu Huan Jin Zheng Qi San (Rectify the Qi Powder Worth More Than Gold)
- Vulnerable cases (elderly and weak): Lian Qiao Bai Du San plus Bu Zhong Yi Qi Tang (Tonify the Middle and Augment the Qi Decoction)
3. Mild Cases: Mild Clinical Symptoms without Neumological Findings from Imaging Studies
A. For adult COVID-19 patients with mild symptoms, in cases with Wind Heat Invading the Lungs, consider Lian Qiao Bai Du San (Forsythia Power to Overcome Pathogenic Influences) plus Ge Gen Jie Ji Tang (Kudzu Decoction to Release the Muscle Layer).
Clinical considerations: Confirm exterior or respiratory symptoms from Wind Heat Invading the Lungs (chills and fevers, or slight chills, weakness, heavy head and body, muscle pain, dry or small amount of phlegm, sore throat, thirsty, but not wanting to drink, no sweat or not feeling refreshed after sweating).
Authors' Commentary:
Ge Gen Jie Ji Tang used in this guideline is a modification of Chai Ge Jie Ji Tang (Bupleurum and Kudzu Decoction to Release the Muscle Layer). Sheng Ma (Rhizoma Cimicifugae) has been added to Chai Ge Jie Ji Tang.4 Ge Gen Jie Ji Tang as used in this guideline consists of the following herbs:
- Ge Gen (Radix Puerariae), Chai Hu (Radix Bupleuri), Huang Qin (Radix Astralagi), Chi Shao Yao (Radix Paeoniae Rubrae), Qiang Huo (Radix et Rhizoma Notopterygii), Shi Gao (Gypsum Fibrosum), Sheng Ma (Rhizoma Cimicifugae), Bai Ji (Rhizoma Bletillae), Jie Geng (Radix Platycodi), 3.75g each.
- Gan Cao (Licorice Root), 1.875g
- Three pieces of Sheng Jiang (Rhizoma Zingiberis Recens)
- Two Da Zao (Fructus Zizyphi Jujubae)
B. For adult COVID-19 patients with mild symptoms, in cases with Cold Damp Invading the Lungs, consider Ge Gen Jie Ji Tang plus Bu Huan Jin Zheng Qi San (Rectify the Qi Powder Worth More Than Gold).
Clinical considerations: Confirm exterior and respiratory symptoms (fever, fatigue, whole-body ache, body aches and pain, cough, phlegm, chest tightness with sputum, chest stuffiness), as well as digestive-system symptoms (inability to swallow, nausea, sticky stool or not feeling relieved after defecating) from cold and damp pathogens.
C. For adult COVID-19 patients with mild symptoms, in cases with Damp Heat Obstructing the Lungs, consider Xiao Chai Hu Tang (Minor Bupleurum Decoction) plus Bu Huan Jin Zheng Qi San.
Clinical considerations: Confirm exterior and respiratory symptoms (low or no fever, slight chills, fatigue, heavy head and body, muscle ache, dry cough with small amount of phlegm, sore throat, thirsty without wanting to drink a lot, no sweat, not feeling refreshed after sweating); as well as digestive symptoms (chest tightness, nausea and belching, watery stools, sticky stools, not feeling relieved after defecating) from heat and damp pathogen.
Editor's Note: Part 2 of this article is scheduled to run in the September issue.
References
- As of April 3, 2020, a pre-proofed version of the Chinese official guideline was available here.
- Assoc. of Korean Medicine: akom.org.
- Chart 3 [Recommendations from the National Council of Korean Medicine Association, Internal Medicine (the Lung Systems), 2nd Edition, published on March 5, 2020, Recommended Traditional Asian Medicine Guideline for the Treatment of COVID-19.] The Association of Korean Medicine, Ed.), 2nd Edition, March 14, 2020, pp. 23-24.
- The Ge Gen Jie Ji Tang in this guideline originates from Ge Gen Jie Ji Tang, and appears in Ho Jon's Tongui Bogam (Treasures of Eastern Medicine), published in 1613.