The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
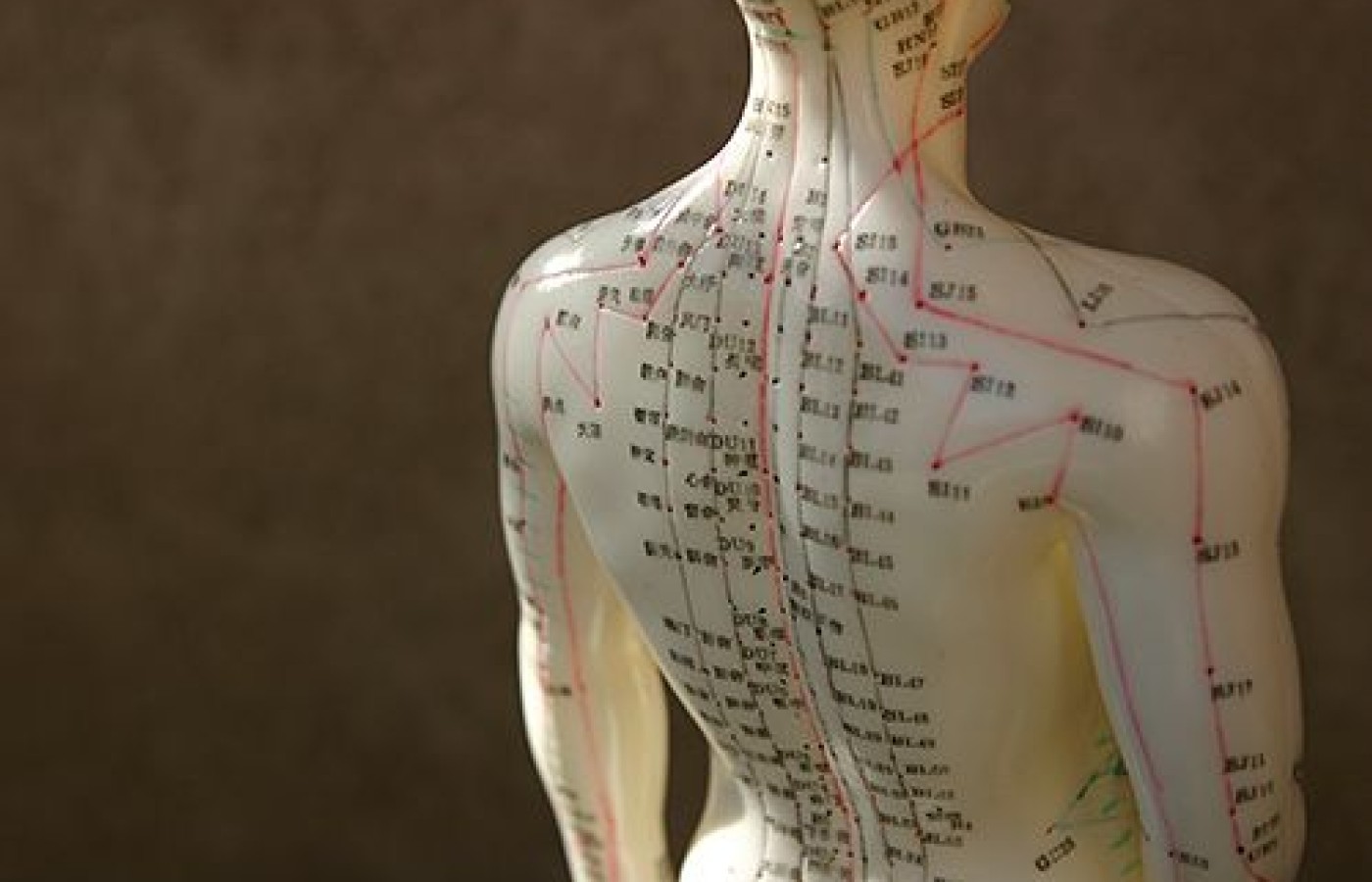
A Common Patient Question: How Does Acupuncture Work?
Acupuncture has a long history—as in 2,500 years long. This means we must respect its many centuries of development. But we must also learn how to explain the origins of acupuncture in a way that works in a modern clinical setting.
When I was in acupuncture school, I took issue with the traditional explanation. It wasn't enough for me to hear the typical "there's qi running through meridians" and "when it gets blocked, it causes pain and disease" spiel. It was surprising to realize that my curriculum lacked a Western/modern explanation on how acupuncture works.
This renders new acupuncturists unable to articulate and communicate the benefits of our medicine to the general public. After doing some research, I discovered how powerful this medicine is. I remember my excitement when I learned the five main mechanisms by which acupuncture stimulates the body. I now use these explanations when one asks the most common question we get, "How does acupuncture work?"
Mechanism #1: Extrasegmental Analgesia
All the way back in 1974, a research group proved that acupuncture increases pain threshold. First, they performed acupuncture on an animal and then injected its cerebral spinal fluid (CSF) into another animal—one that did not receive acupuncture. What was noted was remarkable.
The animal that didn't receive any acupuncture had a higher pain threshold than before.1 This is known as neuromodulation. Neuromodulators are opioid peptides. Four of them have been confirmed to release during an acupuncture treatment.2 One in particular, beta-endorphin, plays an important role in acupuncture analgesia. Studies show that beta-endorphin is released in pain patients receiving acupuncture whereas a control group had no increased numbers of this neuromodulator.3
Mechanism #2: Central Regulatory

Acupuncture also stimulates the deeper parts of the brain, e.g. the limbic system.4-5 Since many of the ways we perceive and respond to pain is the responsibility of the limbic system, this is clearly an essential finding. Perhaps this is why "sham acupuncture" has some therapeutic affect and can possibly cause confusion during research.
Mechanism #3: Local Affects
Two decades ago, it was determined that a neuropeptide called calcitonin gene related peptide (CGRP) get released at the needle insertion site. CGRP causes vasodilation and increases perfusion to the affected local injured tissues. This helps speed up the healing process.6 Studies have found that blood flow increased in individuals as soon as the acupuncture needle was inserted and increased even more when De Qi sensation was attained.7
Mechanism #4: Segmental Analgesia
As we know, pain signals travel via unmyelinated C fibers to the spinal segment and go through the dorsal horn. This is known as the pain or nociceptive pathway. When performing acupuncture near the site of pain or an area innervated by the same spinal segment, we are able to block those pain signals traveling to the dorsal horn. How? Acupuncture stimulates alpha delta fibers which have been shown to decrease the activity in the dorsal horn.8
Mechanism #5: Myofascial Trigger Point Release
Most trigger points develop due to injury (acute or repetitive stress) and tend to develop around the area that is affected. Trigger points have more electrical activity detected by EMG9 which, in turn, causes a release in acetylcholine (ACh). It is the presence of ACh that leads the endplates of a muscle fiber to inhibit the calcium pump. This depolarizes in an uncoordinated way and leads to local contraction of the sarcomeres in the area. As a result, the muscle will shorten.10 By needling the trigger point, it physically disrupts the dysfunctional muscle and causes vasodilation of the area which helps the tissues to heal.
Since learning the types of mechanisms that acupuncture initiates in the body, I use variations of the above details when talking with both my patients and Western health care providers. The traditional explanation has its value but we must be able to cite documented proof of how our medicine works.
My hope is that a clearer understanding of how acupuncture stimulates the body will build bridges between Western and Eastern medicine and move us more towards integration. Such a complementary approach empowers us to give the best possible care to our patients.
References
- Han J. Acupuncture and Endorphins. Neuroscience Letters, 2004 May 6; 361(1-3):258-261.
- Han J, Terenius L. Neurochemical basis of acupuncture analgesia. Annual review of Pharmacology and Toxicology, 1982;22:193-220.
- Clement-Jones V, et al. Increased beta-endorphin but not met-enkeph-alin levels in human cerebrospinal fluid after acupuncture for recurrent pain. Lancet, 1980 Nov 1;2(8201):946-949.
- Hui K, Liu J, et al. Acupuncture modulates the limbic system and subcortical grey structures of the human brain: Evidence from fMRI studies in normal subjects. Human Brain Mapp, 2000;9(1):13-25.
- Hui K, Liu J, et al. The integrated response of the human cerebro-cerebellar and limbic systems to acupuncture stimulation at ST 36 as evidenced by fMRI. Neuroimage, 2005 Sept;27(3):479-496.
- Dawidson I, Angmar-Mansson B. The influence of sensory stimulation (acupuncture) on the release of neuropeptides in the saliva of healthy subjects. Life Sciences, 1998;63(8):658-674.
- Sandberg M, Lundeberg T, et al. Effects of acupuncture on skin and muscle blood flow in healthy subjects. European Journal of Applied Physiology, 2003 Sept;90(1-2):114-119.
- Sandkuhler J. Learning and memory in pain pathways. Pain, 2000 Nov;88(2):113-118.
- Hubbard D, Berkoff G. Myofascial trigger points show EMG activity. Spine, 1993 Oct 1;18(13):1803-1807.
- Mense S, Simons D. Muscle Pain: Understanding Its Nature, Diagnosis and Treatment. Philadelphia: Lippincott Williams, & Wilkins, 1999.
Resource
- Pariente J, White P, et al. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage, 2005 May 1;25(4):1161-1167.