The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
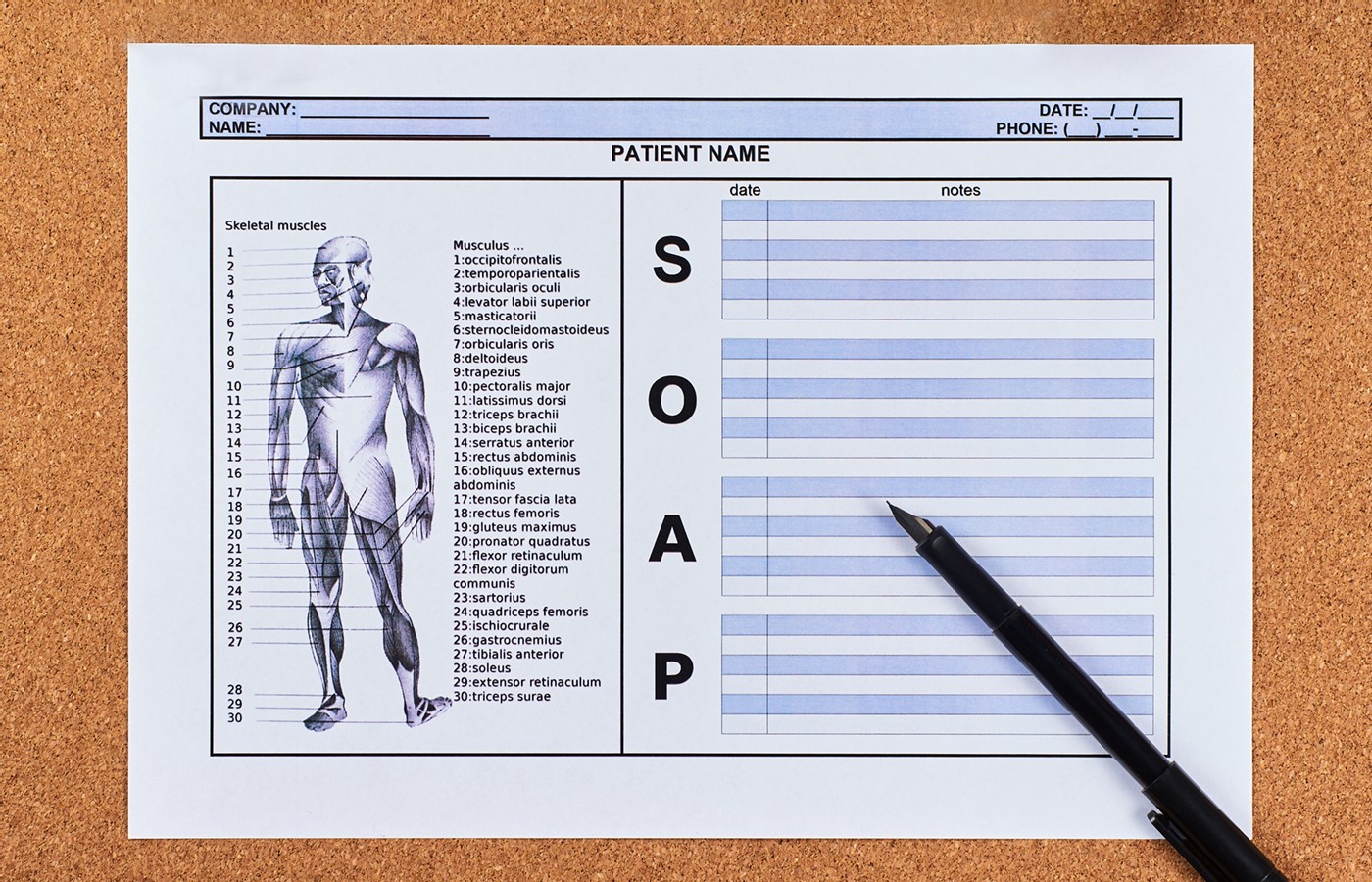
4 Reasons You Should Be Using SOAP Notes
- SOAP notes allow you to quickly locate a patient’s complete health history by creating one place for all their relevant information.
- With the ability to house all patient information in one place, you can then keep better track of patient progress by staying organized, sharing information with other health care practitioners, sharing information with insurance companies, and referencing previous appointments and notes.
- Another significant advantage to moving to electronic SOAP notes is that you can seamlessly integrate with other practitioners on your patient’s health care team.
If you haven’t moved to web-based SOAP notes yet, may I ask: What you are waiting for? Implementing electronic SOAP notes can help you streamline your practice. If you have been reluctant to embrace this technology, there is no better time than today to get started.
Doing some due diligence will help you find robust electronic medical records solutions that offer built-in SOAP note templates. Having these templates built-in allows you to house the record of your examination, assess your patient fully and provide a diagnosis, and then develop a treatment plan you and your patient can follow together that includes medications, therapies, etc.
Don’t let the technology intimidate you. Let’s discuss four great reasons that remove the fear of moving to SOAP notes.
Understanding SOAP Notes
First, it’s essential to define the four components of SOAP notes. Here’s the breakdown:
- Subjective – What the patient says regarding their health issues.
- Objective – This is where you come in. This is the record of their exam and descriptions of their various conditions.
- Assessment – This component summarizes the patient’s diagnosis. If a patient has more than one condition, there might be more than just one diagnosis included in this section.
- Plan – The final component is the treatment plan you, the practitioner, will follow up on. This includes any medications / herbs prescribed, any therapies, procedures, etc.
Now that you understand what SOAP notes are and are not, let’s look at the reasons to move to SOAP notes now.
1. A One-Stop Shop
The first benefit has to do with convenience and efficiency. SOAP notes allow you to quickly locate a patient’s complete health history by creating one place for all their relevant information. With SOAP notes, you can filter through a patient’s clinical history at a glance. You can also add treatment protocols, prescription info and general notes.
All client communication is stored in one simple place you and your staff can access with the push of a button.
2. Treatment Strategies Simplified
As you discuss treatment options with your patients, you can add digital notes directly to their files. You can adjust in real time. SOAP notes programs should allow you to directly add your diagnosis as an ICD-10 code, so you never have to create a treatment plan from scratch.
A robust electronic medical records system will allow you to stay compliant with local insurance payor requirements by utilizing templates that include customizable treatment plans. Using existing templates allows you to streamline your office processes, thus saving you time.
These systems are designed for ease of use and to help with your record keeping and health insurance processing, ensuring patients have their treatments covered by their specific insurance plan.
3. Improved Patient Outcomes
With the ability to house all patient information in one place, you can then keep better track of patient progress by staying organized, sharing information with other health care practitioners, sharing information with insurance companies, and referencing previous appointments and notes.
When a practitioner can keep track of a patient’s progress, including improvements and regressions, it will lead to improved patient outcomes, as you can better track their progress in real time, making any necessary adjustments; with the ability to look back and see what has worked in the past and track changes moving forward.
4. Save Time and Be a Part of the Care Team
All these features allow you to save time, which saves you money and future burnout. Streamlining your procedures gives you many more options for structuring your practice. Do you want to see more patients or spend more time with the patients you already have?
If your billing is a mess, an EMR can help you organize your office back-end, so you have fewer billing errors, thus improving your cash flow and bottom line.
Another significant advantage to moving to electronic SOAP notes is that you can seamlessly integrate with other practitioners on your patient’s health care team. Completing SOAP notes for each appointment allows your patient’s complete care team to understand their condition better and track their progress.
And for practitioners who may be a part of your patient’s care team in the future, your SOAP notes documentation will help to inform them so they can make appropriate treatment choices, thus enhancing the patient’s continuum of care.
Practice Relevance
Your ability to evaluate each of your patients and document their condition appropriately is a critical factor in maintaining excellent care and excellent communication between you and your patient and the rest of their care team. Using SOAP notes ultimately makes it easy to provide your expertise in care and support better outcomes for all your patients.