The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
The Neuroscience of Emotions
- Emotions act as a warning sign to the practitioner, indicating what organs may be involved in a patient’s pattern of imbalance.
- One of my main treatment goals when working with these patients is to calm shen, utilizing areas that are mapped over the vagus nerve.
- While Western Medicine is still in its infancy when it comes to exploring the mind-body-spirit connection, scientific research demonstrates the correlation between the state of the organs, particularly that of the heart, the emotions, and their impact on both physical and mental health.
In traditional Chinese medicine, the “shen,” often translated as both “spirit” and “mind,” lives primarily in the heart organ. The shen is also said to live in the blood, in direct relationship with the heart, the body, and all the organs nourished by the blood. Each of the body’s organs has its own “mind” or aspect of shen, which correlates to an emotion that indicates that organ’s involvement in a pattern. (Figure 1)
Emotions act as a warning sign to the practitioner, indicating what organs may be involved in a patient’s pattern of imbalance. When we think about shen, we think about the emotions, but we also use the word “shen” akin to the way Western medicine would use the word “mental,” or of the mind. It infers a thinking or governing action, as well as an emotional and spiritual nature.
| Lung | Spleen | Heart | Kidney | Liver |
| Grief/Sadness | Worry/Overthinking | Mania/Joy/Anxiety | Fear | Irritability/Anger |
Figure 1: The primary Zang Organs and their corresponding emotions.
Western neuroscience has discovered aspects of the heart that confirm this thousand-year-old Chinese medical concept. Dr. Armour (1991)1 discovered the existence of what he termed a “little brain” within the heart. Research indicates that the heart has around 40,000 neurons, or sensory neurites, that function similarly to brain neurons. This network allows the heart to function independently of the influence of the brain. This means that the heart can likely hold its own memories. Furthermore, the heart is likely capable of learning, sensing, and feeling.2
Dr. Armour describes this network as an “intrinsic cardiac nervous system,” which includes efferent pathways (pathways leading away from the heart) containing both parasympathetic and sympathetic neurons that transmit messages to the brain. This means that the heart can have either an excitatory or a calming effect on the brain, facilitating or inhibiting activity.3 This can be related to the dual TCM concepts of a “calm shen,” wherein a patient is at peace, balanced, able to rest and use energy as needed; and that of a “disturbed shen,” wherein a patient is exhibiting symptoms of mania, anxiety, restlessness, insomnia, or palpitations.
Further research into this connection indicates that the heart sends more information to the brain than the brain sends to the heart. Some examples of information that the heart relays to the brain include sensations, information on heart rate (an increase in heart rate could be due to fear, excitement, or agitation), cardiac cycle timing (some research indicates that stimuli presented during systole may be less noticeable than those presented during diastole), and pain perception.2
Often when working with patients who are dealing with chronic pain, or who are evolving toward chronic pain, the nervous system appears to be incredibly heightened, attuned to even the smallest sensation. These patients appear to be living in a chronic state of fight or flight.
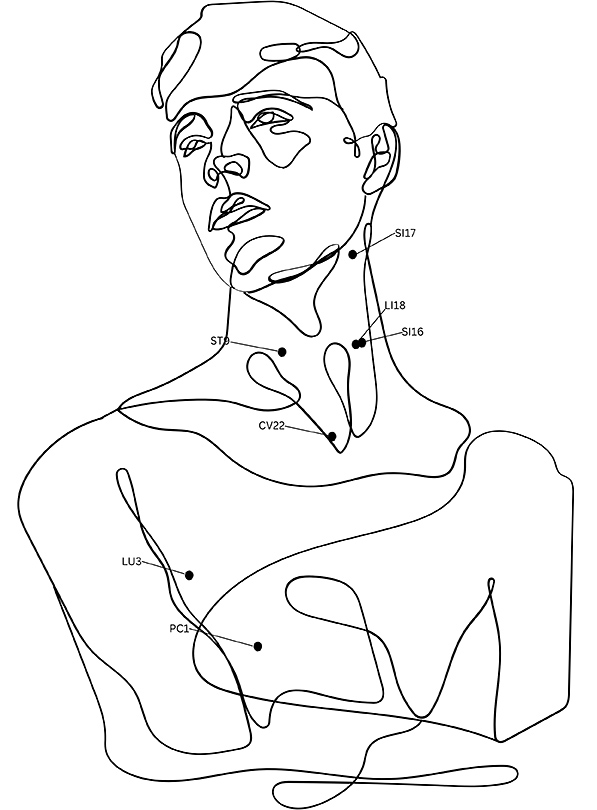
One of my main treatment goals when working with these patients is to calm shen, utilizing areas that are mapped over the vagus nerve, such as the ear microsystem, the upper and middle kidney points, Window of Heaven points (Figure 2), stomach or spleen points on the abdomen, or the Ren channel (including CV 14, the front-mu of the heart). This approach is very helpful clinically when it comes to modulating pain reactions in the brain.
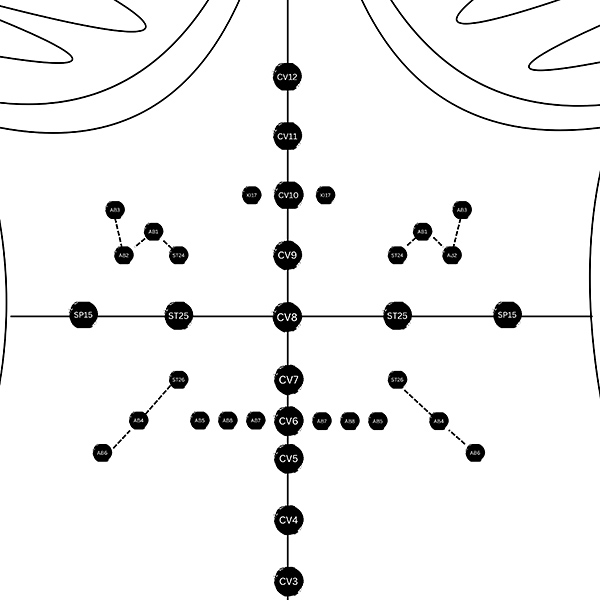
Furthermore, the Abdominal Turtle microsystem (Figure 3), which maps the body on the abdomen using a combination of stomach channel points, kidney points, spleen points, Ren points, and extra points (AB 1, AB 2, AB 3, AB 4, AB 5, AB 6, AB 7, AB 8) has proven to be very effective at combatting chronic pain in clinical practice.
A great deal of the communication between the heart and the brain is accomplished via the vagus nerve, which runs through the ear, the neck, the chest, and the abdomen, enervating the gut, liver, heart, and lungs, transmitting signals back and forth between these areas and the brain.
The areas of the brain that are reached by the vagus nerve include the medulla, hypothalamus, thalamus, amygdala, and the cerebral cortex.1 These areas of the brain are heavily involved in adrenal function, endocrine function, pain perception, and with the autonomic nervous system.
Furthermore, research has demonstrated that “The stimulation of vagal afferent fibers in the gut influences monoaminergic brain systems in the brain stem that play crucial roles in major psychiatric conditions, such as mood and anxiety disorders.”4 In other words, if the gut, liver, heart, or lungs are in a state of imbalance, this information is carried to the brain via the vagus nerve, where mood and mental health are directly impacted.
In TCM the heart is The Emperor, whose job is to rule over the other organs and their emotions and processes in the body. Moreover, the shen is believed to hold a kind of implicit memory, which informs the way that we unconsciously act and respond to stimuli.5 Fright, or trauma, is said to scatter the shen, which can then cease to reside in the heart, creating dysfunction in the body that prevents recovery.
It is often through working with the shen that balance in the body can be restored. Each emotion (Figure 1) is said to injure its corresponding organ, each acting as a fractal of the heart’s shen.
6th-century philosopher, Liu Zhou, said, “If the spirit is at peace, the heart is in harmony; when the heart is in harmony, the body is whole; if the spirit becomes aggravated the heart wavers, and when the heart wavers the body becomes injured; if one seeks to heal the physical body, therefore, one needs to regulate the spirit first.”6 While Western Medicine is still in its infancy when it comes to exploring the mind-body-spirit connection, scientific research demonstrates the correlation between the state of the organs, particularly that of the heart, the emotions, and their impact on both physical and mental health.
References
- Armour JA. Intrinsic cardiac neurons. J Cardiovasc Electrophysiol, 1991;2(4):331-341.
- Alshami AM. Pain: is it all in the brain or the heart? Curr Pain Headache Rep, 2019;23(12):88.
- McCraty R. Influence of cardiac afferent input on heart-brain synchronization and cognitive performance. Int J Psychophysiol, 2002;45(1-2):72-73.
- Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front Psychiatry, 2018;9:44.
- Maciocia G. “Memory in Chinese Medicine,” 2021. Read Here
- Fruehauf H. All disease comes from the heart: The pivotal role of the emotions in classical Chinese Medicine. Classical Chinese Medicine, 2006. Read Here
Additional Resources
- Greenwood MT. A window on protracted neck pain. Med Acu, 2021;33(3): 190-196.
- Huang W, Pach D, Napadow V, et al. Characterizing acupuncture stimuli using brain imaging with FMRI - a systematic review and meta-analysis of the literature. PloS One, 2012;7(4):e32960.
- Salem MO. “The Heart, Mind and Spirit,” 2007. Read Here
- Shipsey, D. (2022, February 1). “Abdominal Acupuncture – A Micro-system With Super Powers.” Eastern Currents, 2022. Read Here



