The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
Does a Torn Rotator Cuff Always Require Surgery?
In a typical year, surgeons in the U.S. perform more than 270,000 rotator-cuff surgeries1 and more than 90 percent of these surgeries involve the supraspinatus tendon.2 Because the average cost of a rotator-cuff repair is about $25,000,3 this translates into almost $7 billion annually for the surgical management of rotator-cuff tears. What's worse, because our population is aging and remaining active, these numbers are expected to increase in the next few years.4
What makes the high surgical prevalence and astronomical expense so frustrating is the fact that studies going back more than 30 years have shown the majority of rotator-cuff tears gradually improve over time, whether treated operatively or nonoperatively.5-7 In fact, research out of Germany8 and Norway9 confirms that partially torn supraspinatus tendons can regenerate following exercise intervention.

Keep in mind that while even large partial tears of the supraspinatus can do well without surgery, massive, full-thickness tears of the supraspinatus occasionally require surgical intervention, especially in young, athletic patients. In most cases, surgery is recommended within the first three months following the development of initial symptoms,10 as the muscle quickly atrophies following complete tendon rupture.
Surgical vs. Nonsurgical: The Research
In one of the few long-term studies comparing the effects of surgical versus nonsurgical care for rotator-cuff injuries, Song, et al.,4 evaluated pain and function at regular intervals over a five-year period in patients receiving operative vs. nonoperative care for large rotator-cuff tears. Interestingly, at the three-month mark, the surgically treated group had significantly worse outcomes, as they reported more shoulder pain and disability than the nonsurgically treated group. However, by 15 months, the surgically treated group had less pain and greater function, which was also true at the two-year mark.
It is important to note there was an 80 percent probability that both groups would achieve a good outcome by 60 months, which is consistent with numerous studies showing good outcomes whether the patient receives surgery or not.7,11

While the majority of orthopedic authorities continue to be baffled by the fact that most patients with supraspinatus tears get better without surgery, they shouldn't be. In 1998, an anatomic study by Minagawa, et al.,12 confirmed that up to 50 percent of the posterior portions of the supraspinatus tendon interdigitate with the superior portions of the infraspinatus tendon (Fig. 1). The shared common fibers create a strain-shielding effect by which the infraspinatus can offload a damaged supraspinatus.
The ability of infraspinatus to offload even a large tear of the supraspinatus was proven in a cadaveric study in 2009.13
This research emphasizes the importance of strengthening the infraspinatus when dealing with a supraspinatus tear, and also explains why the supraspinatus and infraspinatus often tear at the same time.2
The Right and Wrong Way to Test for Degree of Tear
Because massive, full-thickness tears have better long-term outcomes with surgical repair,4 it is important to diagnose the degree of supraspinatus tearing with physical examination. The most common in-office test to identify supraspinatus tears is the Jobe test. This test is performed by having the patient resist abduction in the scapular plane (scaption) while the examiner notes pain and/or weakness.
Unfortunately, the sensitivity / specificity of this test for diagnosing moderate full-thickness tears is poor,14 and many practitioners refer out for more accurate testing such as MRIs and/or diagnostic ultrasonography, which are often cost-prohibitive given the natural tendency for the majority of these injuries to resolve over time.
The easiest way to quantify the degree of supraspinatus tearing without expensive testing is with a simple in-office screening using a handheld dynamometer. This particular test was developed by researchers at Washington University,15 who performed diagnostic ultrasound on 237 subjects to determine the overall health of the supraspinatus tendon.
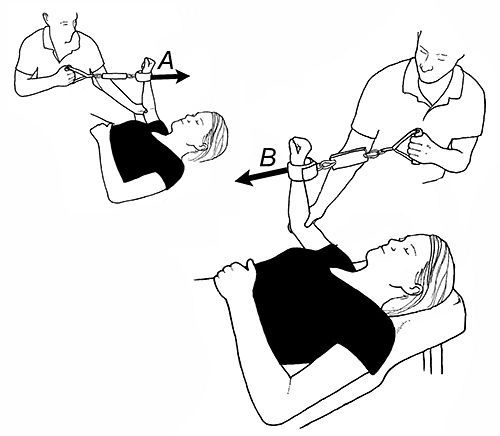
Next, the researchers used a standard dynamometer to measure strength in the shoulder abductors and external rotators; 90° scaption (abduction with the shoulder horizontally flexed 30° to the frontal plane) with the palm down. (Fig. 2) Shoulder external rotation strength was measured with the humerus abducted 0° and internally rotated 45°. The abduction strength score was then divided by the external rotation strength score and if the resultant ratio was greater than .86, the supraspinatus tendon was deemed healthy.

If the strength ratio was approximately .7, the subjects were more likely to have a moderate to significant full-thickness supraspinatus tear. If the strength ratio fell below .48, the subject almost always had a massive, full-thickness supraspinatus tear.
I like this test because it takes about two minutes to perform and supplies important information, not just for determining the extent of the tear (and hence whether or not to refer out for a second opinion regarding surgery), but also for evaluating the response to a rotator-cuff strengthening program.
Handheld dynamometry can also be used to evaluate strength ratios between the shoulder internal and external rotators. Quantifying this ratio is invaluable, as weakness of the external rotators relative to the internal rotators is an extremely common cause of not just supraspinatus tears, but also a wide range of shoulder injuries.
To perform this test, the supine patient is positioned with the shoulder abducted 90° and the elbow flexed 90°. (Fig. 3) A ratio is created by dividing external rotation strength by internal rotation strength. In professional athletes, the strength ratio should be close to one, and in the general population, it should be above .75.16 In a five-year study of professional baseball pitchers, athletes who scored below .75 were significantly more likely to be sidelined with a shoulder injury.17
Exercises to Accelerate Recovery
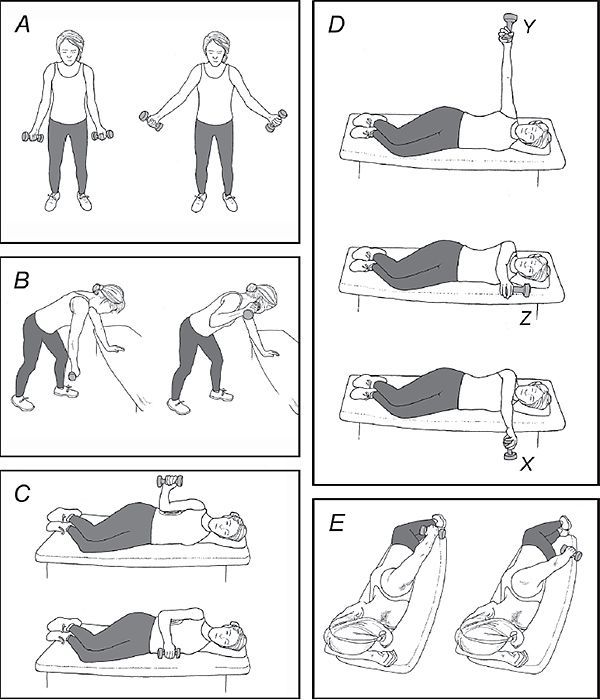
My favorite exercises for restoring the proper internal:external strength ratio are illustrated in Figure 4. Note that these exercises specifically target the supraspinatus and external rotators. A comprehensive rotator-cuff rehab program should include exercises for the entire kinetic chain, including the scapular stabilizers, core and even the lower extremity.
It should be emphasized that while a handheld dynamometer is great for diagnosing the severity of injury, identifying rotator-cuff muscle imbalances and monitoring response to exercise intervention, a growing body of research is showing that manual therapy plus exercise produces better outcomes than either one alone.18 This is especially true for restoring internal rotation, horizontal flexion and/or inferior glide of the humeral head in the glenoid fossa.
In my experience, restoring these specific motions greatly accelerates recovery for all but the worst rotator-cuff injuries, especially when coupled with a thorough exercise routine.
References
- Jain N, Ayers G, Koudelkova H, et al. Operative vs nonoperative treatment for atraumatic rotator cuff Tears: a trial protocol for the Arthroscopic Rotator Cuff Pragmatic Randomized Clinical Trial. JAMA Network Open, 2019;2(8):e199050. doi:10.1001/jamanetworkopen.2019.9050.
- Dunn W, Kuhn J, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity: a cross-sectional study of 393 patients with symptomatic atraumatic full-thickness rotator cuff tears. J Bone Joint Surg U.S.), 2014;96:793-800.
- Lambert L, Bokshan S, Ready L, et al. The primary cost drivers of arthroscopic rotator cuff repair surgery: a cost-minimization analysis of 40,618 cases. J Shoulder Elbow Surg, 2019 Oct;28(10):1977-1982.
- Song A, DeClercq J, Ayers G, et al. Comparative time to improvement in nonoperative and operative treatment of rotator cuff tears. J Bone Joint Surg (U.S.), 2020;102:1142-50.
- Toi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res, 1992 Feb;275:165-73.
- Bokor DJ, Hawkins RJ, Huckell GH, et al. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res, 1993 Sep;294:103-10.
- Khatri C, Ahmed I, Parsons H. The natural history of full-thickness rotator cuff tears in randomized controlled trials: a systematic review and meta-analysis. Am J Sports Med, 2019; 47:1734-1743.
- Jonsson P. Wahlström P, Öhberg L, et al. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc, 2006;14:76-81.
- Torensen T, Meen H, Stiris M. The effect of medical exercise therapy on a patient with chronic supraspinatus tendinitis. Diagnostic ultrasound-tissue regeneration: a case study. J Orthop Sports Phys Ther, 1994;20:319-327.
- Wolf B, Warren R, Wright D, et al. Indications for repair of full-thickness rotator cuff tears. Am J Sports Med, 2007;35:1007.
- Fucentese S, von Roll A, Pfirrmann C, et al. Evolution of nonoperatively treated symptomatic isolated full-thickness supraspinatus tears. J Bone Joint Surg (U.S.), 2012 May 2;94(9):801-8.
- Minagawa H, Itoi E, Konno N, et al. Humeral attachment of the supraspinatus and infraspinatus tendons: an anatomic study. Arthroscopy, 1998;14(3):302-306.
- Andarawis-Puri N, Richetti E, Soslowsky L. Interaction between the supraspinatus and infraspinatus tendons. Effective anterior supraspinatus tendon full-thickness tears on infraspinatus tendon strain. Am J Sports Med, 2009;37:1831-1839.
- Holtby R, Razmjou H. Validity of the supraspinatus test as a single clinical testing diagnosing patients with rotator cuff pathology. J Orthop Sports Phys Ther, 2004;34:194-200.
- Kim HM, Teefey S, Zelig A, et al. Shoulder strength and asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg (U.S.), 2009; 91:289-296.
- Møller M, Nielsen R, Attermann J, et al. Handball load and shoulder injury rate: a 31-week cohort study of 679 elite youth handball players. Br J Sports Med, 2017;51:231-237.
- Byram I, Bushnell B, Dugger K, et al. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. Am J Sports Med,2010;38:1375-1382.
- Pieters L, Lewis J, Kuppens K, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther, 2020;50:131-141.



