The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
TCM for Lyme Disease and Co-Infections
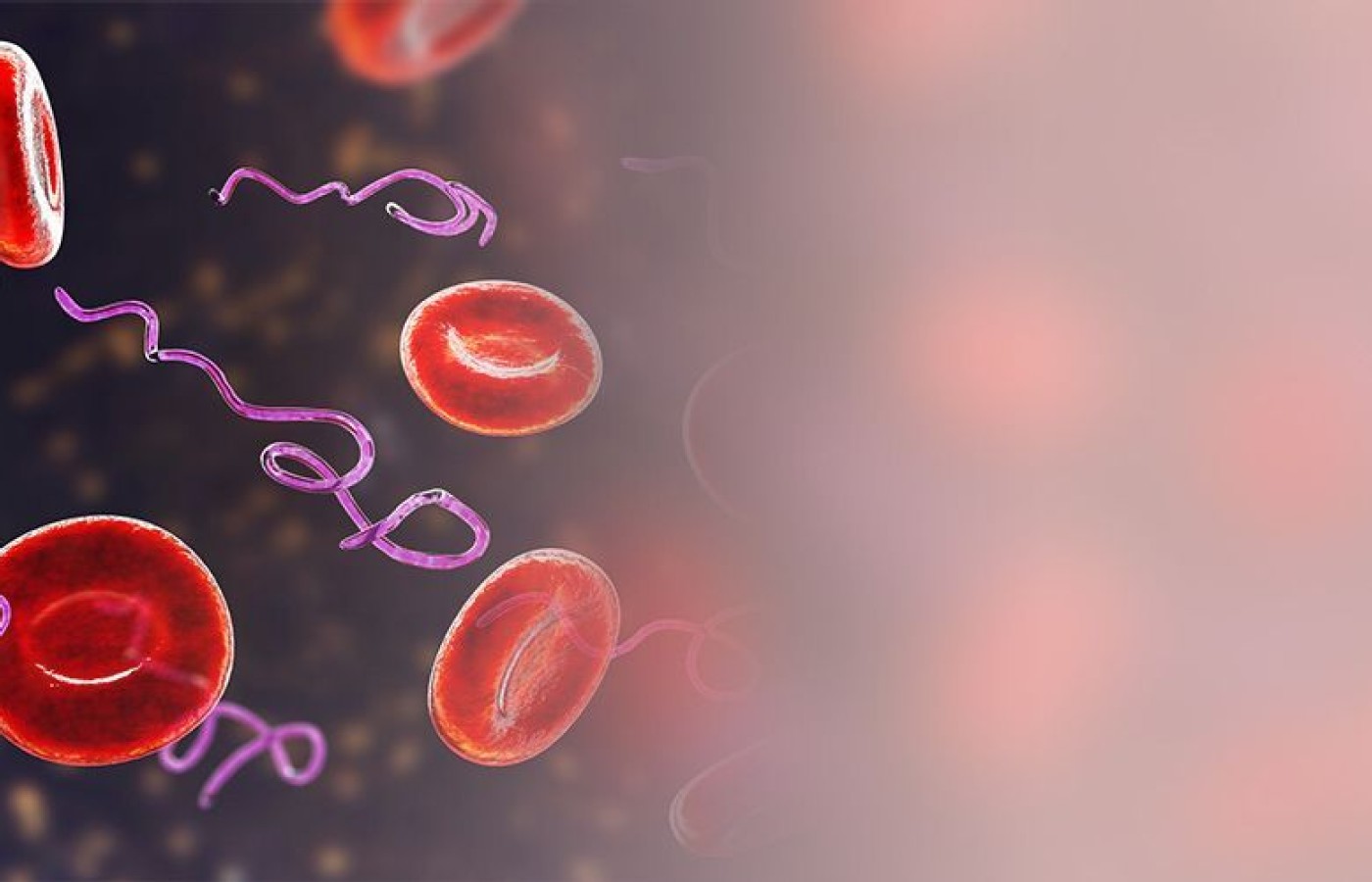
The Lyme disease spirochete, Borrelia burgdorferi (Bb), is one of the most sophisticated bacterium with 853 genes that encode a variety of bacterial proteins for their complexed cellular structure. These proteins can trigger a broad-spectrum immune response which damages multiple organs.
If the infected patient does not get treated promptly and the infection becomes chronic, they can develop symptoms systemically with more severe neurological symptoms. These symptoms include brain fog, feelings of detachment, memory loss, anxiety, panic attacks, agitation, fever, fatigue, insomnia, constipation or diarrhea, burning sensations throughout the body, joint pain, and body pain.
Lyme Neuroborreliosis
According to the International Lyme and Associated Disease Society, up to 40 percent of late-stage Lyme patients develop neurological disorders. Bb can spread from the skin to various secondary organs throughout the body including the heart, joints, and peripheral and central nervous system.
Bb possesses many mechanisms to "hide" from the immune system, which allows it to enter the bloodstream. The exact mechanisms by which the spirochetes travel through and along with the blood and bypass the blood-brain barrier are not known. Some argue for a penetration of the spirochetes between the endothelial cells, whereas others favor a transcellular passage. Once in the cerebrospinal fluid (CSF), the spirochetes elicit an inflammatory response and the aforementioned symptoms occur.1
Co-Infections
Co-infection with other types of microbes is extremely common among late-stage Lyme disease patients. Research of more than 3,000 patients with chronic Lyme disease found that more than 50 percent had co-infections, with 30 percent reporting two or more co-infections.2
The most common co-infectors include nematodes and mycobacteria. This is because instead of being opportunistic pathogens, these microbes may have a symbiotic relationship with spirochetes such as Bb. Co-infection prevents eradication of spirochetes and makes clearing Lyme disease much more challenging, which is why traditional antibiotic treatment fails for so many patients. In order to completely clear the Lyme spirochete infection, treatment that eliminates the symbiotic species is also necessary.
TCM Recommendation
TCM formulas that clear damp heat and cold damp are recommended and have been shown to be effective in clearing not only the Lyme spirochete, but also the co-infections. Tufuling (Rhizoma Smilacis Glabrae) is commonly used in Lyme disease protocols and also treats STDs caused by syphilis (another spirochete, like Bb).3
Jin Yin Hua (Flos Lonicerae) has very strong antibacterial and microbial effects, and is an anti-inflammatory.3 Compared with other commonly seen antibacterial drugs, it exhibits a broader antimicrobial spectrum, more powerful antibacterial activity, and inhibition of drug-resistant bacteria.4
Fang Feng (Radix Saposhnikoviae) is used as a Chinese herbal medicine for the treatment of immune system and nervous system diseases.5 It exhibits significant anti-inflammatory, analgesic, antioxidant, antiproliferative, antitumor, and immunoregulatory activities.5 This is an important factor since Bb disrupts the immune system.
He Shi (Fructus Cnidii) and She Chuang (Fructus Carpesii) are utilized in TCM to warm the kidneys as a way of invigorating yang, expelling cold and wind, eliminating dampness and destroying parasites.6
She Chuang has been used for centuries to kill roundworm parasites such as nematodes.6
Zhe Bei Mu (Bulbus Fritillariae Thunbergii) has beneficial effects for inhibiting mycobacterium, strengthening the immune system and reducing drug resistance.7
Rou Gui (Cortex Cinnamomi) has been shown clinically to have antimicrobial and anti-parasitic activity.8 It also protects susceptible hosts against opportunistic parasites like those in Lyme disease.8
These herbs, in combination other herbal formulas, have been shown to be effective in addressing the Lyme disease spirochete; as well as the co-infected nematodes and mycobacteria. Patients can experience symptom improvement in 2-4 weeks and can achieve significant improvement in three months, based on clinical experience.
During the process of eliminating the Lyme spirochete and other co-infections, die-off effects can occur and make patients' symptoms worse. In order to combat this effect, herbal formulas that clear heat from the kidneys and liver are needed. Ze Xie (Rhizoma Alismatis), for example, helps control inflammatory markers and reduces oxidative stress levels that may be aggravated by the dead parasites.9
Clinical Case: Lyme Disease Solution
— Chrisenia White, ND
A 22-year-old female presented with Lyme disease. Her symptoms were severe joint pain and fatigue, and she was breaking out all over. She had tried multiple treatments up until this point, but never experienced sustained relief. In August, the patient started on seven herbal formulas (Jin Yin Hua, Fang Feng, He Shi, She Chuang, Zhe Bei Mu, Rou Gui, and Tufuling) to help clear the damp heat.
Two weeks into the treatment, her symptoms flared, but then calmed down. She noticed an improvement in her brain fog and fatigue. Her appetite was still low and she was forcing herself to eat.
By the end of December, the patient had finished the low-dose, parasite-killing formulas and she was feeling much better in regards to her brain fog, fatigue and appetite. The patient continued with a kidney yin formula to help clear any residual toxins.
References
- Rupprecht TA, Koedel U, Fingerle V, Pfister HW. The pathogenesis of lyme neuroborreliosis: from infection to inflammation. Mol Med, 2008 Mar-Apr;14(3-4):205-12.
- Johnson L, Wilcox S, Mankoff J, Stricker RB. Severity of chronic Lyme disease compared to other chronic conditions: a quality of life survey. PeerJ, 2014 Mar 27;2:e322.
- Xu S, Shang MY, Liu GX, et al. Chemical constituents from the rhizomes of Smilax glabra and their antimicrobial activity. Molecules, 2013;18(5):5265-5287.
- Li Y, Cai W, Weng X, et al. Lonicerae Japonicae Flos and Lonicerae Flos: a systematic pharmacology review. Evid Based Complement Alternat Med, 2015;2015:905063.
- Yang M, Wang CC, Wang WL, et al. Saposhnikovia divaricata - an ethnopharmacological, phytochemical and pharmacological review. Chin J Integr Med, 2020 Nov;26(11):873-880.
- Zhong J, Liu Z, Zhou X, Xu J. Synergic anti-pruritus mechanisms of action for the Radix Sophorae Flavescentis and Fructus Cnidii herbal pair. Molecules, 2017 Sep 4;22(9):1465.
- Yang ST, Lin YR, Wu MY, et al. Utilization of Chinese medicine for respiratory discomforts by patients with a medical history of tuberculosis in Taiwan. BMC Complement Altern Med, 2018;18:313.
- Ranasinghe P, Pigera S, Premakumara GA, et al. Medicinal properties of "true" cinnamon (Cinnamomum zeylanicum): a systematic review. BMC Complement Altern Med, 2013 Oct 22;13:275.
- Choi E, Jang E, Lee JH. Pharmacological activities of Alisma orientale against nonalcoholic fatty liver disease and metabolic syndrome: literature review. Evid Based Complement Alternat Med, 2019 Jun 3;2019:2943162.