The most important relationship I seek to nurture in the treatment room is the one a patient has with their own body. We live in a culture that teaches us to override pain, defer to outside authority, and push through discomfort. Patients often arrive hoping I can “fix” them, but the truth is, we can’t do the work for them. We can offer guidance, insight and support, but healing requires their full participation.
Dysautonomia: The Medical Condition You May Already Be Treating
TCM practitioners have spent thousands of years healing patients without knowing or needing the names of their diseases as defined by allopathic medicine. We have syndrome names that are both poetic and efficient. But sometimes, an allopathic term helps you administer care and refer a patient more effectively.
Aids, chronic fatigue syndrome and fibromyalgia are examples of new diseases and syndromes, metabolic and contagious that have been discovered/defined over the past few decades. Dysautonomia, like other "new" diseases of the past, is on the rise. In this article, I have excerpted from the Dysautonomia International website. This is a very important resource on the subject and one I hope you take a look at.
What is Dysautonomia?
Dysautonomia is an umbrella term used to describe a malfunction of the Autonomic Nervous system that can result in several medical conditions. Because it is speculated that there are up to four million North Americans struggling with it, to varying degrees and with multiple symptom profiles, because it can be terrifying for patients and their families, because you may be treating people with dysautonomic symptom profiles, and because few physicians know what the disorder is, I want you to be able to identify patients who are candidates for testing. On average, it takes five years for patients to be diagnosed. If you believe one or more of your patients fits a dysautonomia syndrome profile, referring them for the appropriate testing could save years of struggle and possibly, fine tune your treatment plan.

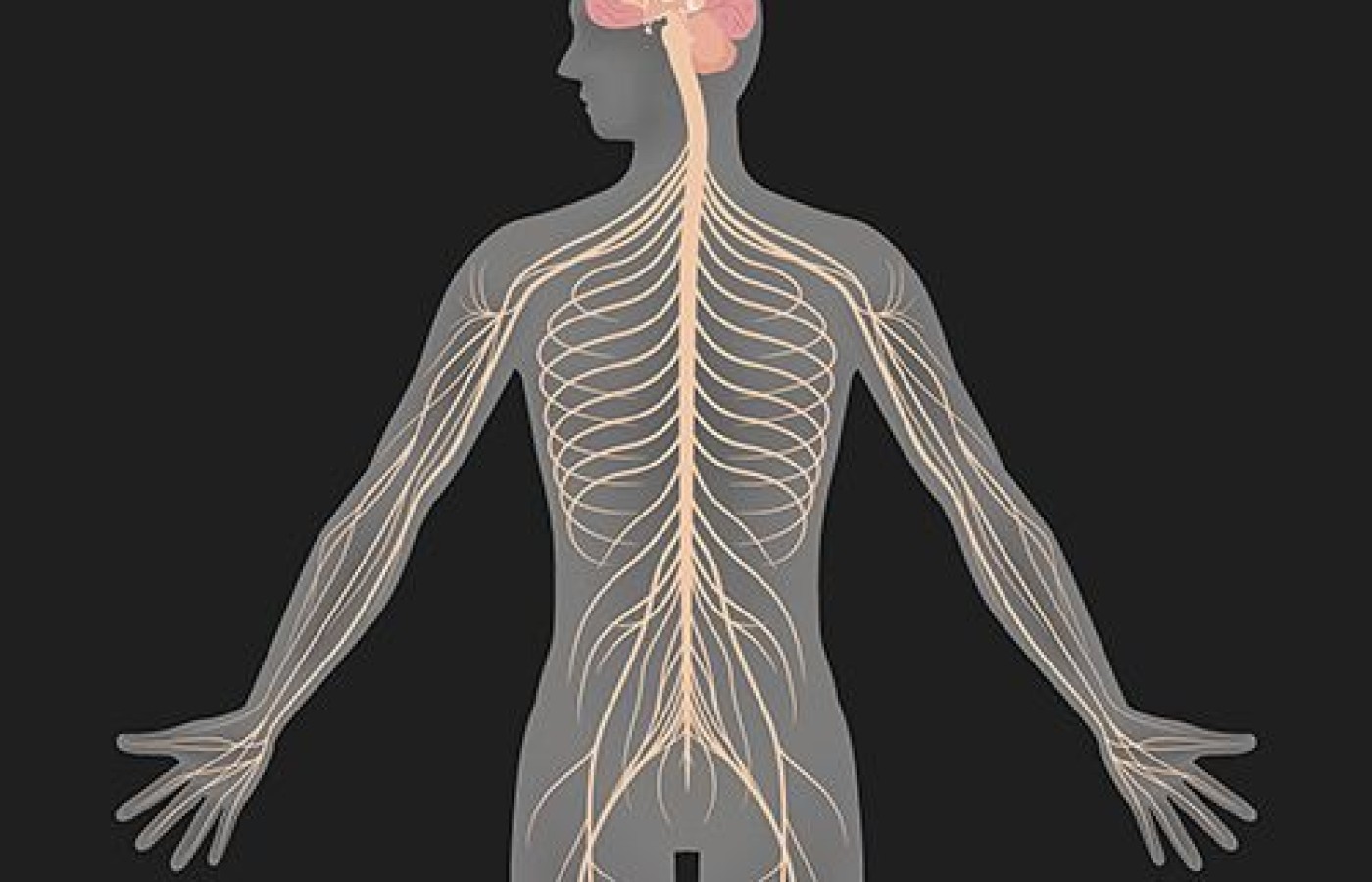
The Autonomic Nervous System controls the "automatic" functions of the body that we do not consciously think about: heart rate, blood circulation and pressure, digestion, dilation and constriction of the pupils, moistening of the eyes, kidney function, and temperature control. People living with various forms of dysautonomia have trouble regulating these systems, which can result in lightheadedness, with or without bending, fainting, fatigue, unstable blood pressure, shortness of breath, dry eyes, abnormal and fluctuating heart rates, panic and anxiety, malnutrition, and in severe cases, death.
More than 70 million people worldwide live with various forms of dysautonomia. People of any age, gender or race can be effected. Some have mild symptoms and can continue normal work, school, social and recreational activities. For others, symptoms may be so severe that normal life activities, such as bathing, housework, eating, sitting upright, walking or standing can be significantly limited. Allopathic medicine can address symptoms but has no cure for any form of the disease at this time.
Causes & Forms
There is still uncertainty as to the cause of the condition. Some types are passed genetically. Other cases occur secondary to other medical conditions, such as diabetes, multiple sclerosis, rheumatoid arthritis, Lyme's, Celiac, Sjogren's Syndrome, Lupus, Parkinson's and other autoimmune disorders. Many patients also have TBI, traumatic brain injury. Some seem to get it for no reason at all.
Postural Orthostatic Tachycardia Syndrome (POTS) is estimated to impact 1 out of 100 teenagers and, including adult patients, a total of one million to three million Americans. A common expression of dysautonomia and a form of orthostatic intolerance (symptoms exist upon standing and disappear upon reclining) POTS predominantly impacts young women of childbearing age who look healthy on the outside, though there are male patients. Researchers compare the disability seen in POTS to the disability seen in conditions like COPD and congestive heart failure.
POTS patients may experience fainting, fatigue, headaches, lightheadedness, heart palpitations, (what we would call shen rising and plum pit chi in the chest and throat) exercise intolerance, nausea, diminished concentration, digestive upset, shaking, coldness or pain in the extremities, chest pain and shortness of breath. A percentage of patients develop a reddish purple color in the legs upon standing, believed to be caused by blood pooling or poor circulation. The color change subsides upon returning to a reclined position. The symptoms can be many or few, intense or mild, depending upon the individual.
Neurocardiogenic Syncope (NCS) is the most common form impacting tens of millions of individuals worldwide. Many have a mild case, with fainting spells once or twice in their lifetime. However, some individuals have severe NCS, which results in fainting several times per day, leading to falls, broken bones and sometimes traumatic brain injury. Individuals with moderate to severe NCS have difficulty engaging in work, school and social activities due to the frequent fainting attacks.
Multiple System Atrophy (MSA) is a fatal form of dysautonomia occurring in adult ages 40 and up. It is a neurodegenerative disorder with similarities to Parkinson's, but unlike Parkinson's patients, MSA patients usually become fully bedridden within two years of diagnosis and die within 5 to 10 years. MSA is considered a rare disease, with an estimated 350,000 patients worldwide.
Your Practice
Many dysautonomia patients look healthy. They may be any age and addressing another chronic disease. Do not let a patient's healthy appearance fool you. These are sick people, even if their symptoms are not severe. Dysautonomia can look like many other conditions regularly seen in your office: mood swings, anxiety, emotional overwhelm and low stimulation tolerance, fatigue, chest tightness, fainting or dizziness, headaches, depression, multiple miscarriages, dry eyes, etc.
We listen very carefully to patients' pulses. When dysautonomia is involved, it is wise to consider if pulse emptiness is caused by abnormally low blood pressure that is part of this condition. Do you take blood pressure readings? It's a good idea to do that with every patient. I suggest you take patients blood pressure once they have quieted their bodies and are lying on your treatment table. Then take it again, immediately upon their standing. Take it a 3rd time after they have stood for a full five minutes. If you notice drops, that could lead you to consider this condition. As for stability of heart rate, if you check a patient's heart rate several times, even just a few minutes apart, do you notice beat per minute differences? Has a bpm gone from 70 to 90 or from 78 to 65? Dysautonomia patients are known to have heart rate gains or losses of 10, 20, even 50 beats per minute when the pulses is repeatedly taken a few minutes apart, even when the patient is laying perfectly still on your table.
If someone who already has a diagnosis of dysautonomia comes to your practices, get an accurate reading of all their medications. Some patients are on blood pressure raising medications, which can lead an acupuncturist listening to pulses to believe that more chi exists in the organ or channels than is truly the case. It is easy to over treat someone on blood pressure raising medication because of the appearance of an abundance of chi. Those who are not on medications may be taking salt tablets to serve the same purpose. Many patients are on beta-blockers to slow heart rate. While this can help the dizziness and anxiety brought on by tachycardia, it will make their actual heart rate impossible to read in the pulse.
Other patients are on antidepressants; especially those who have experienced traumatic brain injury and those whose limited abilities have lead to depression. Yet others are on medications to address autoimmune disorders. Simply put, learn about the medications these patients are on and recognize that a patient's pulse/tongue will not necessarily be an honest representation of what is going on in the body. Also, check the tongue for wind and inflammation in the system that might have been brought on by the use of medications.
Diagnosed
Dysautonomia can be diagnosed with blood pressure monitoring, checking heart rate fluctuations, and a Tilt Table Test. Considering referring your patient for this test if she has repeated, unexplained episodes of fainting or dizziness or if these symptoms exist upon standing but not while lying. A tilt table test may be appropriate if a patient has fainted only once, because another episode could put them at high risk of injury.
During a tilt table test, the patient lies flat on a table. Straps are put around the body to hold it in place. After about 15 minutes of lying flat, the table is quickly tilted to simulating a change in position from lying down to standing up. The table will then remain upright for up to 45 minutes, while heart rate and blood pressure are monitored. This allows doctors to evaluate the body's cardiovascular response to the change in position.
Perhaps patients have described this symptom to you. They wake in the morning and have pain. After taking a few steps or moving about with morning tasks, the pain dissipates and they are pain free for the rest of the day. This type of pain is related to chi deficiency stagnation. Without external movement, the body cannot keep it's own chi moving sufficiently to avoid stagnation resulting in pain upon initial movement. But with more external movement, the symptoms go away. A Tilt Table test works the same way. While a patient may frequently go from sitting to standing without passing out or feeling dizzy, the test limits their ability to move so all the chi to raise blood pressure and move blood must come from inside the body. A positive test results would involve dizziness or even fainting. I have had patients pass out cold during these tests, even though they don't loose consciousness getting out of bed or off the couch.
In the past, POTS was mistakenly believed to be caused by anxiety. However, researchers have determined that POTS is caused by a malfunction of the patient's autonomic nervous system. The anxiety associated is a side effect of tachycardia, elevated heart rate. As many acupuncturists treat anxiety and panic disorder patients, it is especially important to be aware of dysautonomia as a physiologic, rather than psychiatric, cause for this problem.
As mentioned, there is no cure for dysautonomia in allopathic medicine, but secondary forms may improve with treatment of the underlying disease. There are some treatments available to improve quality of life, both with medications and lifestyle changes/adaptations, but even using all treatments available, many dysautonomia patients experience disabling symptoms that significantly reduce their quality of life.
While being aware of this condition and referring patients out for diagnostic and symptom regulating support can be a powerful step in their healing, what we have to offer can also be dramatically helpful. Though no research exists at this time to document the efficacy of acupuncture and herbal medicine in the treatment of dysautonomia, patients have been known to improve. This condition is deep within the body so expectations for quick or even comprehensive recovery should be addressed. High patient compliance is important but as many have been sick for years, their gratitude for progress tends to inspire compliance. They are often desperately searching for anyone who can help.
I found diagnosis like phlegm blocking the channels (to the brain) and blood stasis to be common diagnosis of this problem. But other syndromes are involved. The spleen is often weak and, as the adrenal/pancreatic system is overworked, the kidneys play a role. While there is much to be discussed regarding TCM diagnosis of dysautonomia, you must do a comprehensive exam, as you always do, note the syndromes that you find and treat them. But also consider that dysautonomia may already be in your practice and send patients out for allopathic diagnosis. There are medical centers around the country that specialize in this increasingly common disorder. Patients can benefit by a multi-disciplined approach.